|
Epinephrine (adrenaline) has been a hallmark of cardiac arrest management as an attempt to obtain a return of spontaneous circulation (ROSC). However, the evidence for epinephrine in out-of-hospital cardiac arrest (OHCA) as well as in the hospital (IHCA) has been conflicting. We review the largest trial to date just recently published in the New England Journal of Medicine (NEJM).
Title:
Perkins, et al. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest NEJM July 18, 2018 Case: You are called to the home of a 64 y/o female who suddenly collapsed after reporting chest pain to her spouse. Family called 911 and initiated bystander CPR while waiting for fire and EMS to arrive approximately 8 minutes later. After providing high-quality CPR and defibrillating for ventricular fibrillation, ROSC has not yet been achieved. As the team leader, you start considering if epinephrine should be administered after this initial shock. Background: There has been a lot of debate on the potential risks and benefits of epinephrine for cardiac arrest, but there has been a demand for a large RCT to help answer the question. Epinephrine has been a part of cardiac arrest protocols since the 1960s. Its alpha-adrenergic effects of constriction increases aortic diastolic pressure (what is needed for increasing coronary blood flow) to help increase the chances of ROSC but at the cost of impairing microvascular blood flow including to the cerebral cortex. Also, the beta-adrenergic effects of epinephrine can cause dysrhythmias, increased myocardial oxygen demand, and increases the risk of recurrent cardiac arrest. Clinical Question: Is epinephrine beneficial in the treatment of out-of-hospital cardiac arrest? Reference:
Author’s Conclusions: In adults with OHCA, the use of epinephrine resulted in a significantly higher rate of 30-day survival than the use of placebo, but there was no significant between-group different in the rate of a favorable neurologic outcome because more survivors had severe neurologic impairment in the epinephrine group. Quality Checklist for Randomized Clinical Trials:
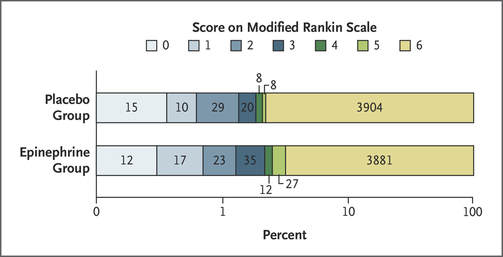
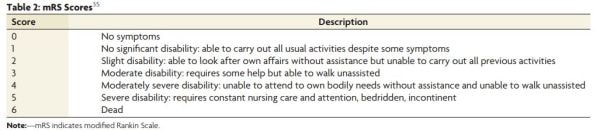
Key Results: A total of 10,623 patients were screened for eligibility for which 8103 were randomized (trial pack opened) and 8016 were enrolled in the trial (pack opened and drug administered). 4015 patients received epinephrine while 3999 received placebo. Only 7 total patients (3 from the epinephrine group and 4 from the placebo group) were excluded from the primary outcome. 130 patients (3.2%) in the epinephrine group and 94 (2.4%) in the placebo group were alive at 30 days (unadjusted odds ratio for survival 1.39; 95% confidence interval [CI], 1.06 to 1.82; P=0.02) with a fragility index of 6. In regards to discharge from the hospital with a favorable neurological outcome (modified Rankin scale [mRS] of 3 or less) was 87 of 4007 patients (2.2%) in the epinephrine group) and 74 of 3994 (1.9%) in the placebo group but was not statistically significant (unadjusted odds ratio, 1.18; 95% CI, 0.86 to 1.61). A mRS of 4 or 5 was considered severe neurological impairment and at hospital discharge 39 of the 126 patient (31.0%) in the epinephrine group had this versus only 16 of 90 (17.8%) in the placebo group. Key Points of Debate:
Comparing Conclusions: Although more patients will achieve ROSC with epinephrine in OHCA, it does not lead to a significant increase in neurologically intact survival. Our Bottom Line: Epinephrine for OHCA should not be routinely used in cardiac arrest unless higher level evidence can demonstrate its benefits for improving a neurologically intact survival. Resuscitation efforts should still focus on high-quality CPR and early defibrillation. The recognition and correction of reversible causes is also important. Further studies could investigate other medications or dosings, but the focus must be on neurologically intact survival. Case Resolution: After a quick discussion with your team, you all agree to focus on high quality CPR and continued attempts at defibrillation. On the rhythm check, you see an organized rhythm and have a palpable pulse. Your team immediately starts post-resuscitation care and transfers to the closest facility. Clinical Application: At this time, multiple studies have demonstrated that epinephrine may improve ROSC but not neurologically intact survival in OHCA. You can see an extensive list at REBEL EM where they also have a recent review of this trial. Although guidelines still have epinephrine listed in their protocols we must seriously consider limiting its use (if at all) and work to help change guidelines. What do I tell my patient? With your patient in cardiac arrest, you will not be able to talk to them directly but can talk to their family. You explain to the family present that you are working on saving their loved one and that you are using the current best evidence to make that happen. In that time you explain the importance of high-quality CPR and early defibrillation whenever possible. You also explain that sometimes other treatments can be performed which may help but that this is very much on a case-by-case basis. Conclusion: As one my expect, there has been quite a bit of reporting on this topic. In addition to the REBEL EM post mentioned above EMNerd, St. Emlyn's, and First10EM have all made posts. Check these out but make sure to read the article yourself! Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
1 Comment
|
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||



 RSS Feed
RSS Feed