|
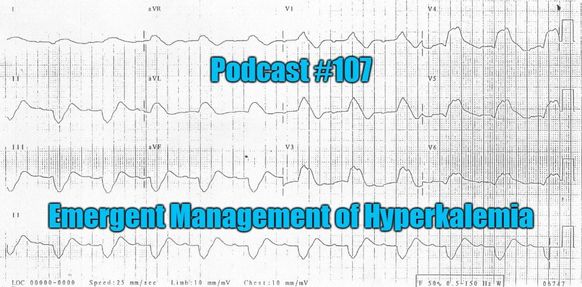
We see changes in potassium levels all of the time in patients. However, what works and what does not? What is the evidence behind the management? Are there special pearls? These questions and much more are addressed in this podcast with Michelle Perkins.
Intro—Why Worry?
Emergent Treatment
Treating the Underlying Problem
Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed