|
Intraosseous (IO) devices are traditionally used in the initial stages of resuscitation when peripheral intravenous (IV) access is not readily obtainable. This can happen for a variety of reasons such as edema, burns, obesity, or IV drug abuse among others. Although ultrasound can be used to obtain peripheral or central venous access, the most rapid route is the IO. The device has been used both in adults and children with great success. It can safely facilitate the delivery of fluids, medications, and blood. There are very few contraindications and it is rare to have a complication.
First, before we discuss the IO further, please check out Practical POCUS at PracticalPOCUS.com where you can find out more about the educational group. There are upcoming courses and they are offering a special "early bird" discount.
There is a great systematic review available that covers many of the details on the basics of IOs. The main contraindications are skin infection at the site of insertion, fracture of the bone used (or potentially proximally), severe bone disease, osteogenesis imperfecta, osteoporosis, osteomyelitis of the bone involved, compartment syndrome to the extremity, prior surgery, burns to the area involved, or recent failed attempt at the same bone. Although rare the major complications are compartment syndrome due to fluid extravasation, skin infection, and osteomyelitis. However, there have been rare complications up to death from sternal access due to injuries or the heart or aorta. Mediastinitis is another potential complication seen with older devices. Fat emboli has been questioned but in certain studies this was found in animals both with and without IO access. There are a variety of devices but the EZ-IO is very simple to use with multiple approved sites (except for the sternum). The five signs that indicate correct placement are loss of resistance on entering the marrow cavity, ability of the needle to remain upright without support, bone marrow or blood easily sampled using a syringe, administration of 2ml of saline without tissue swelling, and easy administration of 8ml of saline without resistance. When it comes to drawing blood off of the IO, this is possible and is the main portion of our discussion today. In a 2010 study, there was a significant correlation for many labs. The RBC, hemoglobin, and hematocrit counts in the CBC profile were the same but WBCs and platelets did not correlate. Glucose, BUN, creatinine, chloride, total protein, and albumin in the chemistry profile were well correlated but sodium, potassium, CO2, and calcium concentrations were not. However, sodium was within 5%, calcium within 10%, and the rest were within 25%. With these differences, the WBC is elevated and both CO2 and platelets are low in the IO compared to IV. There are several important limitations of that study. It was small with only 10 healthy volunteers, was all drawn from the humeral site, and it being unknown if the lower CO2 level would have changed with evaluation of arterial blood.
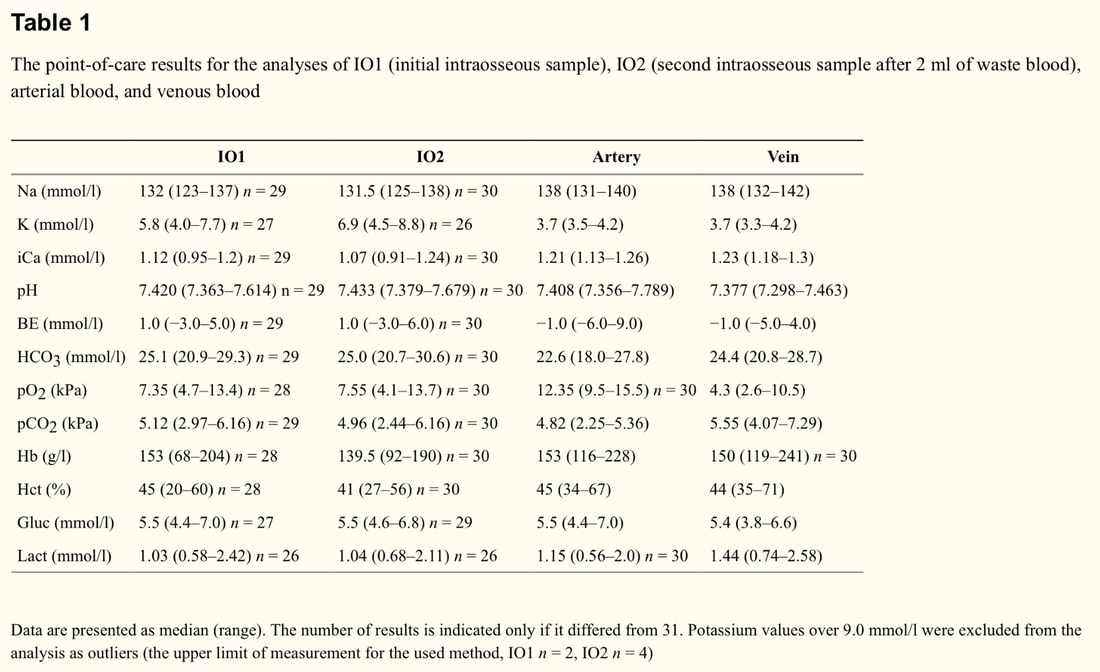
A recent study in 2017 regarding point of care (POC) analysis was used to find agreement between IO and arterial analyses. Again, the EZ-IO was used and i-STAT devices were the POC testing system. Like the previous study, IO was tested twice with before and after wasting but with similar results (the exception being for potassium and hemoglobin). They also tested both arterial and venous blood samples. In this study with 31 healthy participants the potassium levels were found consistently elevated compared to peripheral blood. Sodium and ionized calcium were also slightly lower. IO samples also demonstrated higher results for base excess and bicarbonate. CO2 and O2 levels for the IO fell between arterial and venous lab values. Hemoglobin, hematocrit, glucose, and lactate levels all had good agreement with arterial and venous blood. Again, the study has limitations given its small sample sizes (but larger than anything else) and that the labs could be deranged in critically ill patients compared to healthy patients. Future studies addressing these issues is needed.
It is important to secure the IO device in an appropriate manner. EZ-IO has a standard securing device available. After its use is completed, the IO is removed using a sterile luer lock syringe cane be connected to the hub of the needle for easier grip and then rotated clockwise while pulling. Then, a sterile dressing is applied similar to that with a peripheral IV.
Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed