|
Although point of care ultrasound (POCUS) is a valuable tool, there are times that a formal radiology performed ultrasound is needed. We continue our October POCUS month marathon with a discussion on this topic and how we can improve success for our radiology colleagues. Mainly, we want patient's to have a properly sized bladder that will allow for the best imaging on transabdominal pelvic ultrasound.
As we have mentioned on previous posts, Practical POCUS has upcoming courses in Missouri at the end of the year. With a special discount code "TOTALEM" you can get 10% off! Remember to register soon since there is an early bird discount already in place and the limited seating is filling quickly.
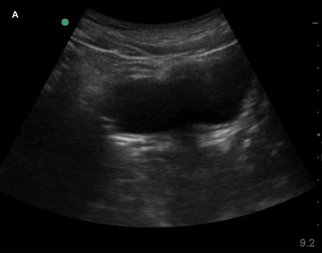
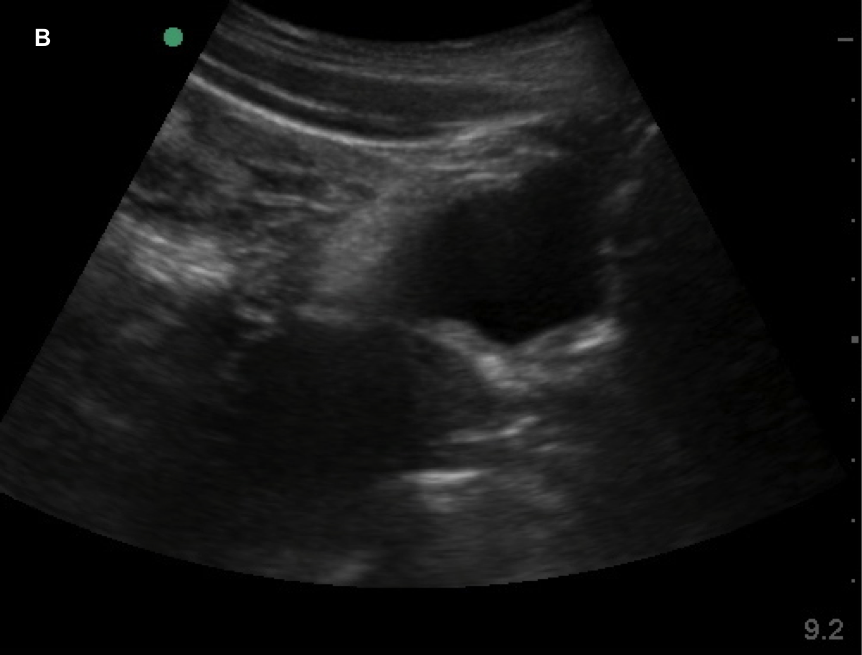
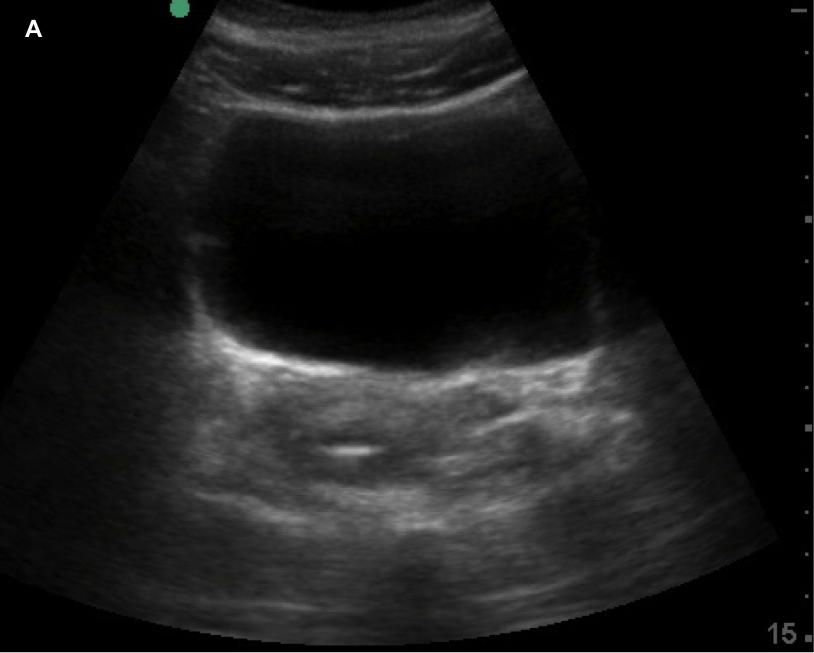
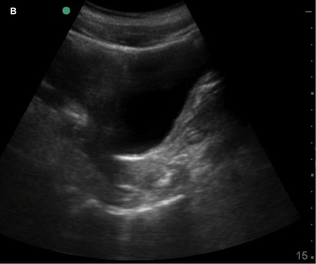
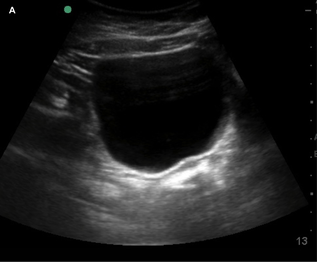
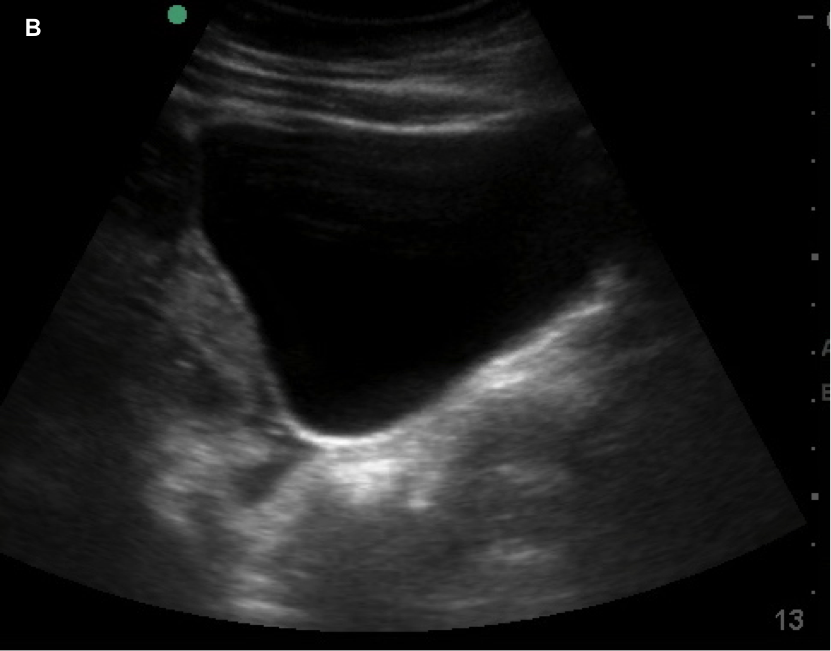
Currently, certain facilities use subjective sensation of bladder fullness to determine patient readiness for radiology performed transabdominal pelvic ultrasound. This is to help adequately visualize the ovaries and uterus. Potentially, POCUS allows for more rapid identification of a patient's readiness for radiology performed ultrasound. This is important due to the need to assess for high-acuity pelvic pathologies such as ovarian torsion, ectopic pregnancy, ruptured ovarian cyst, and tubo-ovarian abscess. In the Annals of Emergency Medicine a recently published paper by Dr. Dessie et al called Point-of-Care Ultrasound Assessment of Bladder Fullness for Female Patients Awaiting Radiology-Performed Transabdominal Pelvic Ultrasound in a Pediatric Emergency Department: A Randomized Controlled Trial covered this very issue. Note, as the title says above this was in a pediatric population but adults would have similar findings. In adults, facilities may use a predetermined size such as bladder width or volume. The width though can be less reliable since even a small bladder can be wide. In the case of pediatric patients though, width and volume will vary by age especially in the enrolled population of females ranging 8 to 18 years of age. To address this issue, patient's bladders were assessed on a qualitative basis. They made three categories as small (minimally distended or collapsed), medium (moderately distended or rectangular), and large (fully distended or ellipsoid). The categories are demonstrated in images listed below.
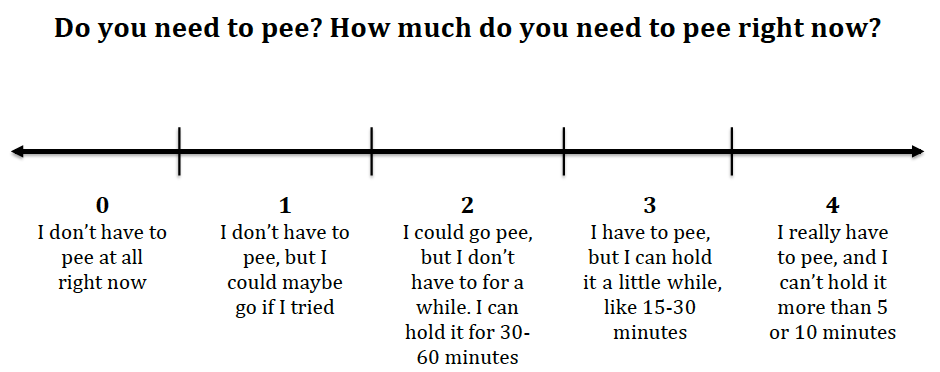
In the usual care group, the patients the endpoint was for patients with a bladder fullness sensation of 3 or 4 (description below of scale). In the POCUS group, the endpoint was visualization of a large bladder or they reached maximal sensation (4 on the scale). Patients were assessed every 30 minutes until the endpoint was reached.
120 patients were randomized with half being in the usual care group and the other half having POCUS exams. All patients assigned to POCUS had successful pelvic ultrasound on the first attempt compared with 84.7% in the usual care group. 25% of all patients with a bladder fullness score of 2 or less had a large bladder on POCUS. The usual care arm's median time to ultrasound was 139 minutes whereas POCUS was 87.5 minutes with an absolute difference of an impressive 51.5 minutes.
There were certain limitations such as the convenience sampling of patients. Although some patients were enrolled overnight by physician researchers in some cases, research assistants were only present from 7 AM to 11 PM. Given the subjective nature, the next potential limitation is the risk of bias in interpreting POCUS images based on the patient's feedback from the scale above. This could have led to over- or under-estimation. Randomization should have helped with some other potential limitations such as the availability of the bedside ultrasound machine at times (since there was only one), transport to the radiology department, and availability of the ultrasound technician. This is also more pragmatic given that these are obstacles many departments must address. The last main limitation is that more than half of all participants in the trial were enrolled by a single researcher which could limit generalizability. POCUS is quick with bladder exams taking less than two minutes. This practical exam that is rapid and easy to perform. It can save a significant amount of time for the patient, staff, and for flow through the department. Some may suggest the use of bladder scanners but these only give a gross volume and do not assess the bladder shape. In the cases of pathology, it also cannot differentiate from other cystic structures. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||||


 RSS Feed
RSS Feed