|
If you have worked in emergency medicine for any length of time, you have seen an abscess. No, it's not a spider bite, it's almost always an abscess. With abscess management, there are a number of approaches. We are going to review a relatively evidence based approach to treating these pus filled pockets of joy. Grab your eye protection and masks as this can get messy.
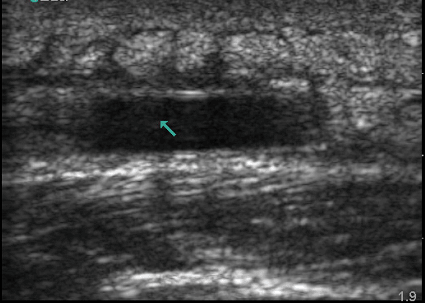
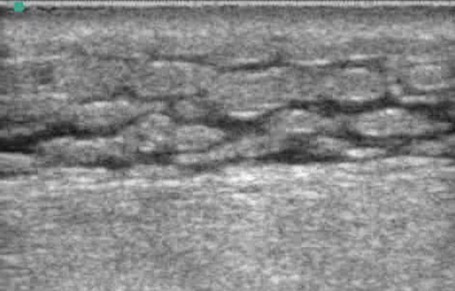
These two images from Mount Sinai EM Ultrasound's page shows an abscess and cellulitis, respectively. On ultrasound, the goal is to find the pocket of fluid called an abscess. The "cobblestone" appearance on the second image is seen with cellulitis. When looking back at the first picture, some of this can also be seen there. Bedside ultrasound can be incredibly beneficial when trying to distinguish between abscess and cellulitis. It is also helpful to look for any potential complications from incision and drainage (I&D) which is the treatment of choice for most abscesses. A scalpel in the wrong place can cause a lot of unwanted problems.
Sometimes with abscesses, people may elect to not have the I&D but use only antibiotics. This is usually only for small abscesses and after a detailed discussion by both the clinician and the patient. There is a lot of debate when this is brought up as cold hard steel with I&D is the classic approach, but is seen on occasion that someone may try to only use antibiotics without the actual procedure. More on antibiotic management though below. What is needed to perform an I&D may depend some on the person performing the procedure but these are classically included:
Packing may not be as beneficial as some thought based on studies such as this one which was also covered by The SGEM here. The same goes for irrigation also discussed in a recent study which The SGEM covered. Ultimately, as discussed in the podcast, both packing and irrigation are being used less often with a few exceptions. Once the supplies are gathered, local anesthesia is used. Also in the same SGEM post covering packing, there was a discussion about using buffered lidocaine based on a Cochrane Review. Lidocaine with epinephrine and its safety has been reviewed in rather great detail with REBEL EM doing an excellent job in this post. One great benefit with lidocaine that contains epinephrine is that it will last longer. It will also help decrease bleeding based on vasoconstriction. Injecting in a grid pattern around the abscess seems to be very beneficial and will help when the abscess is drained as squeezing the area is often required. When performing the I&D, usually an 11 blade is preferred given the stab incision. It is also wise to get the culture early if doing it at all given that it will usually get less messy. Forceps can help break up the abscess as needed. Irrigation may be beneficial as a small amount to help see if everything has been removed, but not necessary especially in large amounts. 10cc of normal saline is often more than enough after adequate removal of the pus. An alternative to traditional packing has been the LOOP technique covered by ACEP here and also on PEMBLOG here. It is a promising technique but still very new. Once the pus has been removed and whatever technique (if any) for packing or for allowing further drainage, cover the area. Antibiotics have been a hot topic for debate. On SGEM 131 there was discussion of this paper comparing clindamycin to trimethoprim-sulfamethoxazole (TMP/SMX) which found no benefit. However, in the most recent SGEM post, a newer paper demonstrates benefit. Both EM Nerd and REBEL EM have also covered this study. There is supposed to be another paper coming out soon favoring antibiotics based on preliminary findings, but this is still pending actual publication. However, this new paper will most likely be covered in the future. Overall, TMP/SMX seems to be of benefit for patients. For other details and to hear an overview, listen to the podcast. Remember to share on Facebook, retweet on Twitter, and rate on iTunes to help spread the word on TOTAL EM. As a side note, if you are interested in joining the project, email at [email protected] or send a message from the page. Thanks to The SGEM for spreading the word of TOTAL EM. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
3 Comments
Fritz PA-C
10/22/2016 10:47:25 pm
Great discussion of an everyday practice. I have become a fan of the loop technique as I think it is less torturous on the patient, their wallet and our colleagues. I also advocate wall suction and Yankauer for those big heroin abscesses! Talan's NEJM article changed my practice on ABX for abscesses. If you can drop subsequent I&D by an absolute of 5.2%, new skin infections on the same patient (who always asks how to prevent this) by 7.2% and infections in household members by 2.4% without harming the patient - why wouldn't you? Well apart from EM Nerds righteous contention that the actual study population had somewhat larger abscesses, DM and fevers - just the group most of us would have added an ABX to regardless. The point is for those "simple" abscesses (that I'm my mind were always < 5CM without any of the above factors) I will now strongly consider ABX for the secondary benefits. Keep up the good work.
Reply
Chip Lange
10/27/2016 03:11:32 am
Thank you! I meant to add suction to the list and glad you brought it up here. Glad you could share your thoughts.
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed