|
A relatively recent article, the SHoC-ED trial, can sound like the need for ultrasonography in hypotension is not necessarily beneficial. In this podcast the trial, along with its strengths and limitations, will be reviewed.
Previous papers such as theSasmaz et al. paper published in Emergency Medicine International in 2016, "Effect of Focused Bedside Ultrasonography in Hypotensive Patients on the Clinical Decision of Emergency Physicians" demonstrated a significant increase in the diagnostic accuracy of why the patient is hypotensive 60.6% before POCUS to 85.0% after POCUS. Furthermore, in that study it led to a change in management for 50% of the 180 patients in the study.
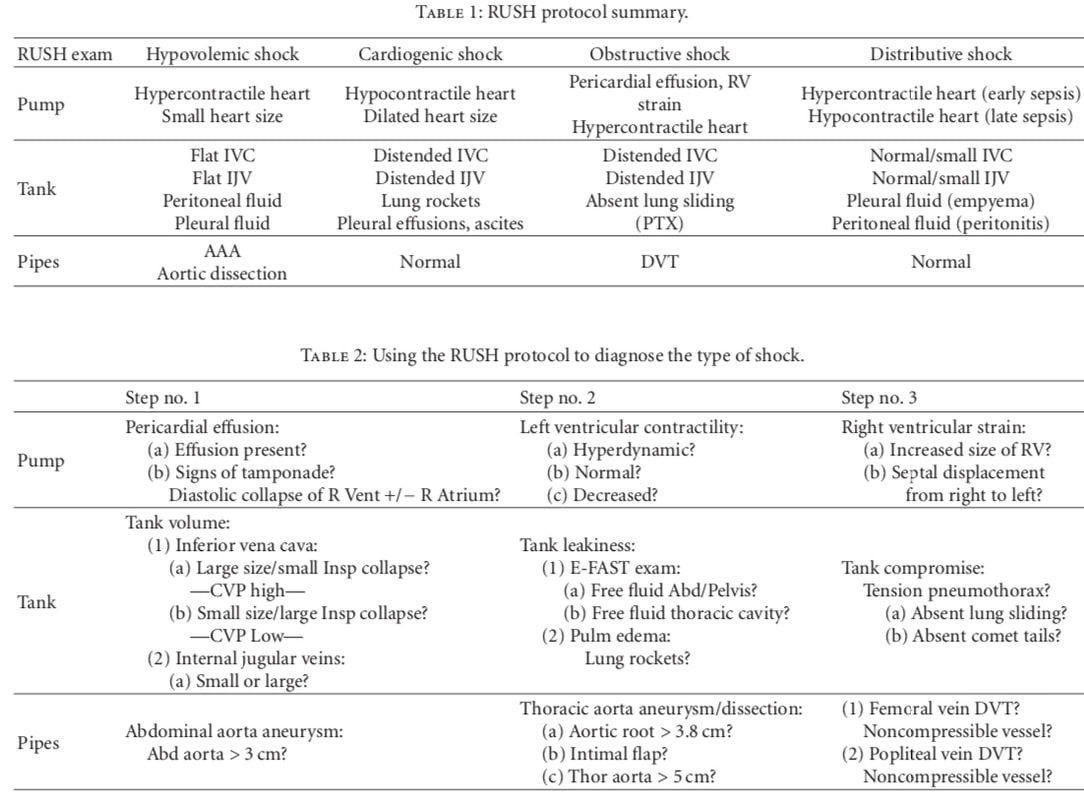
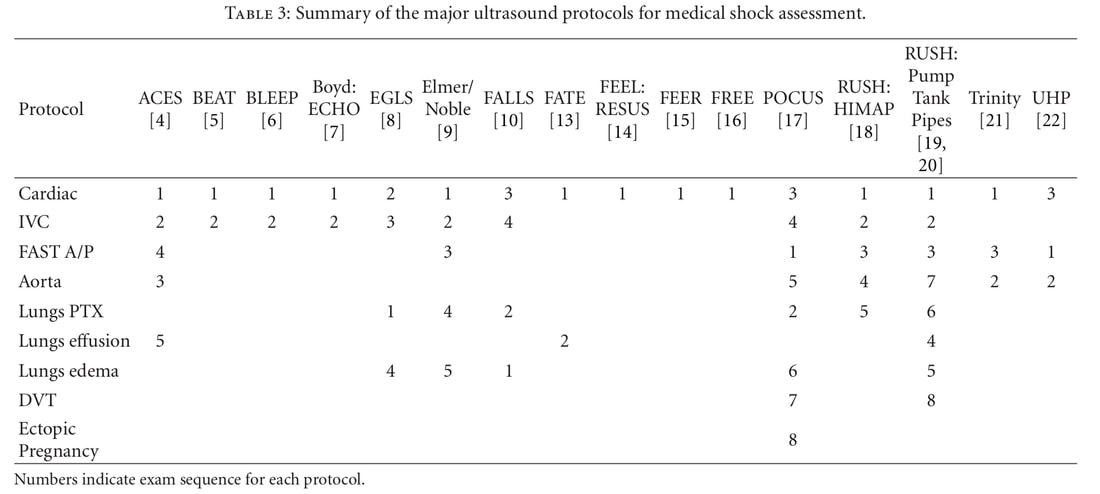
Ultrasound can help identify many important causes of hypotension such as cardiac dysfunction, ruptured aortic aneurysm, and evaluation of fluid status. Probably the most common assessment, the Rapid Ultrasound for Shock and Hypotension (RUSH), exam investigates other potential causes such as pulmonary embolism or pneumothorax. A comparison of the different exams used in undifferentiated shock can be found by Seif et al. published in 2012 in Critical Care Research and Practice. There are essentially two versions of RUSH with one using HI-MAP and the other being the "Pump, Tank, Pipes" approach (PDF for latter below). The review article has some great tables (as shown below) to help identify and differentiate causes of shock as well as explain the differences between the various exams that exist.
Now that we understand the benefits and general undifferentiated shock POCUS exams, let us discuss the SHOC-ED trial. This study looked at patient oriented outcomes primarily survival at 30 days or hospital discharge. Patients were randomized into either a POCUS arm within 60 minutes or a no POCUS arm.
Examination:
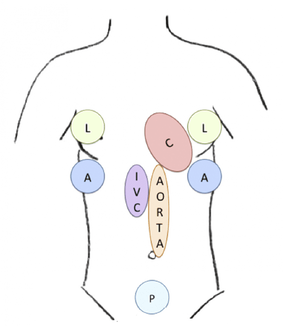
This version of the exam is essentially a HI-MAP exam with evaluation added for pleural effusion. A diagram of the actual protocol is shown below. There is a cardiac (C) exam of the subxiphoid, parasternal long, parasternal short, and apical views. The presence or absence of pericardial fluid was noted as well as the left and right ventricular function and size. The lung (L) exams were for evaluation of pneumothorax and pleural effusions. The right and left upper quadrants (A) were assessed for abdominal free fluid in the hepatorenal and splenorenal areas, respectively. The pelvis (P) was assessed in transverse and longitudinal planes for free fluid and to estimate bladder filling. The IVC was assessed for size and collapsibility. The aorta was measured in a transverse and longitudinal plane with assessment for aneurysm.
Population:
Patients 19 and older with either a sustained systolic blood pressure (SBP) <100 mm/Hg or a shock index of >1.0 with a SBP <120 mm/Hg were included. However, patients who were pregnant, required CPR or ACLS interventions, significant trauma in the past 24 hours, diagnostic EKG for acute myocardial infarction, outside transfer, vasovagal syncope, normal hypotension, or an obvious cause for the hypotension were excluded. Results: The most common category of shock was non-cardiogenic at 87.6% with the most common diagnosis being sepsis (52%). The primary outcome found survival at 30 days or at hospital discharge was 76.5% in the early POCUS arm and 76.1% in the standard care arm. There was no difference in the secondary outcomes measured including rates of CT scanning, inotrope use, intravenous fluid use, ICU admissions, or total length of stay. Strengths: This study addressed a clinically important and patient oriented outcome. It was multi-centered and even international with competency standards compared to the different groups in the study. Very few patients were lost to follow up. There was good allocation concealment. Independent and blinded chart review was performed and the baseline demographics as well as the vital signs were similar between the groups. Limitations: There is specific mention of a "clear cause of shock" as an exclusion criteria, but it would be interesting to have known how many times POCUS changed the diagnosis (as supported by the literature above). Additionally, what is considered a "clear cause" and based on whose observation? Is this a junior level resident or attending physician? The exclusion criteria also includes patients with pregnancy or EKG, but what if these had not been obtained initially? POCUS can play a role for such patients and help guide the evaluation as well as the care given. As for inclusion criteria, it only says sustained hypotension but does not specific for what length of time. Was this just needing repeat blood pressures or a specific time frame? With so many patients having sepsis, POCUS does not directly distinguish this from other pathology. Some findings can help support sepsis causing shock (such as signs of hypovolemia), but it plays a more limited role compared to other causes of shock. Additionally, many of the types of patients removed from this study would carry findings that POCUS is better at catching (such as ectopic pregnancy and trauma). A small number of the remaining patients had findings that POCUS is great for including 2 patients with dissection, 7 patients with venous thromboembolism, 22 patients with left ventricular dysfunction and/or myocardial infarction, and 2 patients with cardiac effusion/tamponade. This was also a convenience sample which carries its own limitations. Additionally, there was no evaluation of those performing POCUS to have their images reviewed and see if they were performing it correctly or missing (or misdiagnosing) pathology. There was no algorithm for what and how to use the images for evaluation and management. Also, POCUS scans could be delayed by 60 minutes meaning that for the time before then (as we saw up to 50% of the time management will change based on POCUS findings) the patient is receiving incorrect care which can impact the benefits of POCUS and early correct management. We need to hit study design itself. This was a small study needing 400 patients (stopped early) to provide an 80% power to detect a reduction in mortality of 10% assuming 30% mortality in the control group. None of this was achieve as the study was stopped early due to poor recruitment and futility. The mortality in the control group was far less than the 30% needed. Additionally, a 10% reduction is large and even a 5% reduction (NNT of 20) would be extremely beneficial. However, a different way to argue the mortality issue is that POCUS is diagnostic and not therapeutic. To expect POCUS to affect 30 day mortality may be a cognitive fallacy. This is further supported by lack of documentation as to how any POCUS findings changed management. We know from previous evidence how POCUS was used much earlier, changed the diagnosis, and changed the management of patients. We are less certain if this is the case here. Paul Atkinson, the lead author, has mentioned many of the above before (in comments on both REBEL EM and The Bottom Line) but does add some additional points. The patients were excluded because they all would receive POCUS and it would be unethical to not have these patients receive such an exam. Additionally, the diagnostic accuracy was 94% in the clinical (control) group which would be very difficult to improve upon with POCUS. This is much higher from previous studies. He did mention that POCUS did not cause harm and that it still plays a role to answer specific quetions. Summary of Study: While this study does not show a clear benefit of POCUS in survival, it is too limited. The study was too small and the mortality rate was not high enough to show the difference as the study was designed to evaluate. It had a significant exclusion list and other limitations. Essentially, this study should not change practice and POCUS should still be considered an important tool in undifferentiated shock and hypotension. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||||||||


 RSS Feed
RSS Feed