|
As point of care ultrasound (POCUS) continues to expand in roles, the diagnosis of appendicitis using POCUS is one application with growing evidence. This is especially true for the pediatric population. In this blog and podcast learn how to diagnose appendicitis by POCUS and some of the most recent evidence.
There are three main imaging modalities to diagnose acute appendicitis: ultrasound, CT, and MRI. MRI is not practical in many situations due to cost and time. It is especially not helpful in the rural and remote environments where such machines may not even exist. CT has been the standard in many ways but the radiation is of concern, especially in the pediatric and pregnant populations. Ultrasound is fast, reliable, and avoids the concern of radiation.
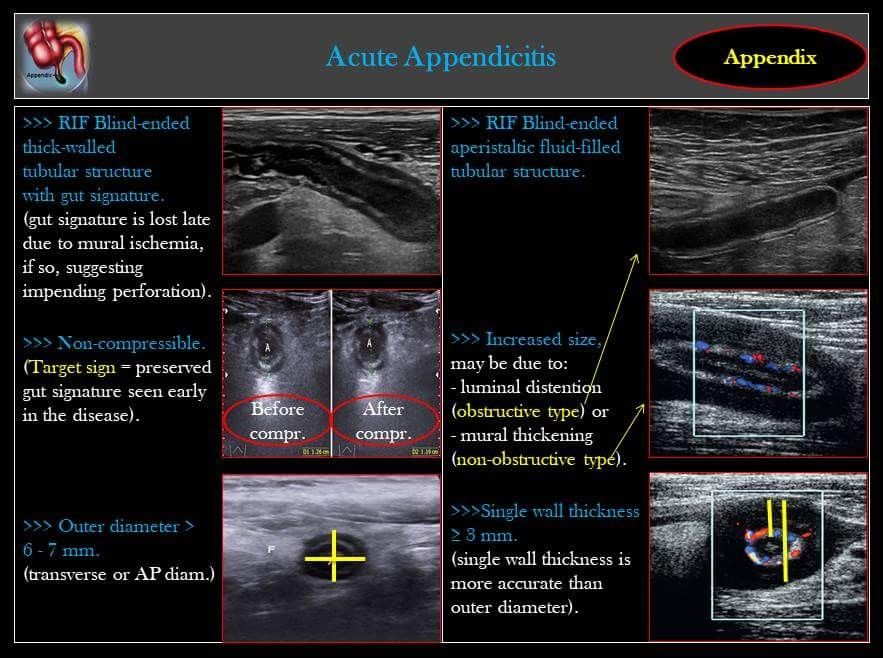
The appendix can be difficult to visualize, especially if it is normal. A blind-ended tubular structure that can contain fluid is what is normally observed for the appendix. During appendicitis, the walls become thickened (>2mm for single wall), the overall size increases (usually considered >6mm), it is non-compressible ("target sign"), and can have a "ring of fire" appearance from increased vascular blood flow. See the diagram below for some of the main details.
We know what we are looking for, but what is the evidence that those working in emergency medicine are good enough to perform the exam? A recent study by Lee and Yun in the American Journal of Emergency Medicine, 2019 titled "Diagnostic Performance of Emergency Physician-Performed Point-of-Care Ultrasonography for Acute Appendicitis: A Meta-Analysis" investigated this very concern. It found that the diagnostic performance by both emergency medicine and radiology was excellent with emergency medicine being even better for pediatric acute appendicitis. In that study, they recommended an outer diameter cutoff of 7mm.
Here are the numbers:
There are some limitations to remember when reading results such as these:
Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed