|
We talk about point of care ultrasound (POCUS) frequently, but a common favorite topic is the use of ocular ultrasound. This application can provide a vast amount of information quickly and easily. As an added bonus, our main paper discussed in this post used PAs. The week this is being originally posted is National PA Week.
Two quick announcements:
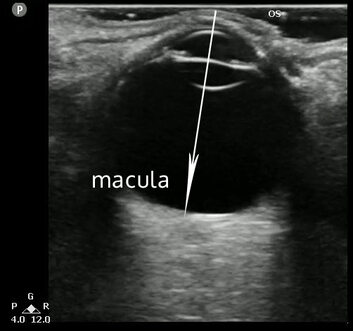
1. Happy PA Week! 2. If you want to learn more about ultrasound check out Practical POCUS, an ultrasound education company For POCUS lovers, it seems like ocular ultrasound was meant to be: a superficial structure that contains mostly fluid. It is easy to see, safe, and can significantly improve the diagnosis of pathology compared to the current standard. Access to ultrasound continues to increase while access to other ways to evaluate eyes like slit lamps are often becoming more difficult to find. Ocular ultrasound can be used to identify a number of serious conditions including retinal detachment, lens dislocation, vitreous detachment and hemorrhage, increased optic nerve sheath diameter, and retained foreign bodies. Below is an example from The POCUS Atlas of a retinal detachment.
Sometimes it can be a challenge to get good data, but the JAMA study published earlier this year was well done and included physicians, residents, and PAs. The paper is titled Point-of-Care Ultrasonography in the Diagnosis of Retinal Detachment, Vitreous Hemorrhage, and Vitreous Detachment in the Emergency Department and was published April 12, 2019 in JAMA. It is open access so make sure to check out the article and review the literature for yourself.
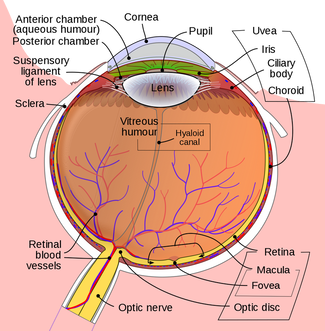
Their clinical question was how accurate is point-of-care ultrasound for diagnosing retinal detachment (RD), vitreous hemorrhage (VH), and vitreous detachment (VD)? This is a great question to ask since it is difficult to examine without specialized equipment and this is a prime use for ocular ultrasound. This was a multicenter, prospective, observational, convenience sample with emergency department patients at four sites: two academic and two country hospitals. All sites had EM residents, ophthalmology residents, and an emergency ultrasonography fellowship. Patients were enrolled between 8 AM and 12 AM by research assistants and POCUS was performed by the treating clinician prior to consultation with ophthalmologist. The ophthalmologist was blinded to POCUS results and more than one diagnosis could be reported. The POCUS diagnoses were then compared to final diagnosis by ophthalmologist after examination Inclusion criteria included symptoms suspicious for RD, VH, or VD (blurry vision, flashes, floaters, vision loss) and having ophthalmologic consultation. Exclusion criteria were when there was no ophthalmologic consultation, the patient was younger than 18 years old, the patient was non-English or non-Spanish speaking, patient declined enrollment, there was incomplete data, or most importantly ocular trauma or suspicion for globe rupture was present. This is a quick reminder that if globe rupture is suspected to avoid ocular ultrasound as this can make matters worse. There were 75 clinicians in the study with five of them being PAs. It may not be a large number, but the fact that they were included in the mix speaks volumes in the progression of emergency medicine and ultrasound literature. The physicians, residents, and PAs came with variable POCUS experience and training. However, all of them received 30 minute lecture and 30 minutes hands-on scanning on healthy volunteers. The pathology was defined by the authors as follows: Retinal Detachment: bright echogenic membrane tethered to optic disc but separated from choroid. Posterior vitreous detachment: detached, thin, mobile membrane at interface between vitreous and retina. Vitreous hemorrhage: fluid collection of variable echogenicity in posterior chamber that rotated with kinetic examination. With a total of 225 patients with a mean age of 51 years old and 40% being women they found pathology in 36% of them. 20.8% had RD, 24% had VH, and 15.1% had VD. Retinal detachment had a sensitivity of 96.9% (CI 80.6-99.6) with a specificity of 88.1% (CI 81.8-92.4). Vitreous hemorrhage had a sensitivity of 81.9% (CI 63-92.4) and specificity of 82.3% (CI 75.4-87.5). Vitreous detachment had a sensitivity of 42.5% (CI 24.7-62.4) and a specificity of 96% (CI 91.2-98.2). Overall, these were great results! It is worth remembering this is a convenience sample with no interrater reliability. Although multi-center in design 173/225 (76.8%) were from one center, with 34, 14, and 4 from the other centers. Given the high prevalence of disease, this actually is helpful for what can be rare pathology. Lower specificity for retinal detachment was seen compared to prior studies. A recent metaanalysis shows 94.2% sensitivity and 96.3% specificity, although lower accuracy if only looking at ED studies. The lower specificity seen in the current study could be based on the protocol, the machines, the training, or maybe its just that a larger study was able to give us a better answer. With this data we must consider the next steps. How do we come up with a more patient oriented outcome such as fewer conversions to macula off detachments or improved outcomes in other forms? There has been minimal evidence regarding the accuracy of POCUS for determining macula on versus off retinal detachments which can change the disposition of patients. The ultrasound image below depicts the location of the macula on ultrasound and is from a case from Ultrasound of the Week. Next to it is the anatomy of the eye for better understanding.
As a final take away, it is worth noting that although these numbers are great, they are not perfect and once again POCUS may be a better tool to rule in pathology. When such pathology is seriously considered to be present we should involve our ophthalmologist colleagues.
Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed