|
Point of care ultrasound (POCUS) can range in complexity from very basic exams to those that are expert level in nature. While some basic wall motion abnormalities are taught in many introductory classes, the concept of regional wall motion abnormalities (RWMA) for myocardial infarctions (MIs) can be a little more complicated and as a result is often not taught to novice learners of POCUS. Some have questioned the validity of the results, as well. In this post, we will cover some highlights including recent evidence that may further support the potential role of RWMA in MIs.
While the heart is contracting we should see the walls thicken. The way to think about RWMA is that a section of a wall of the heart is not moving like the rest of the heart when those walls are supposed to be contracting. It stands out from the rest by either moving less (hypokinesia), not moving at all (akinesia), or moving in the opposite direction as the rest of the wall (dyskinesia).
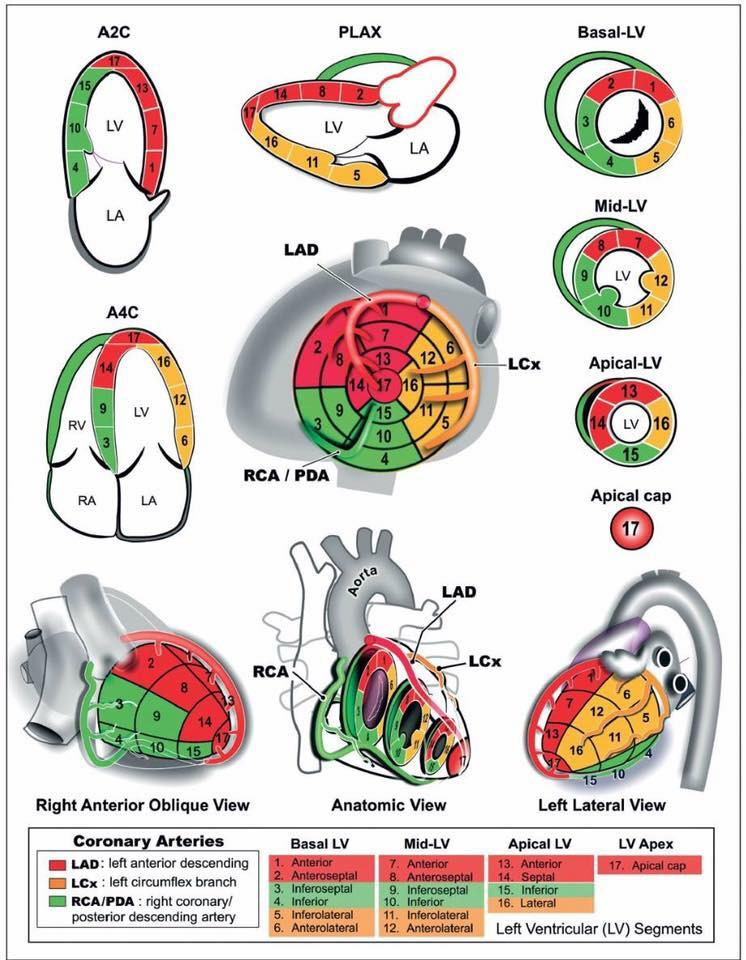
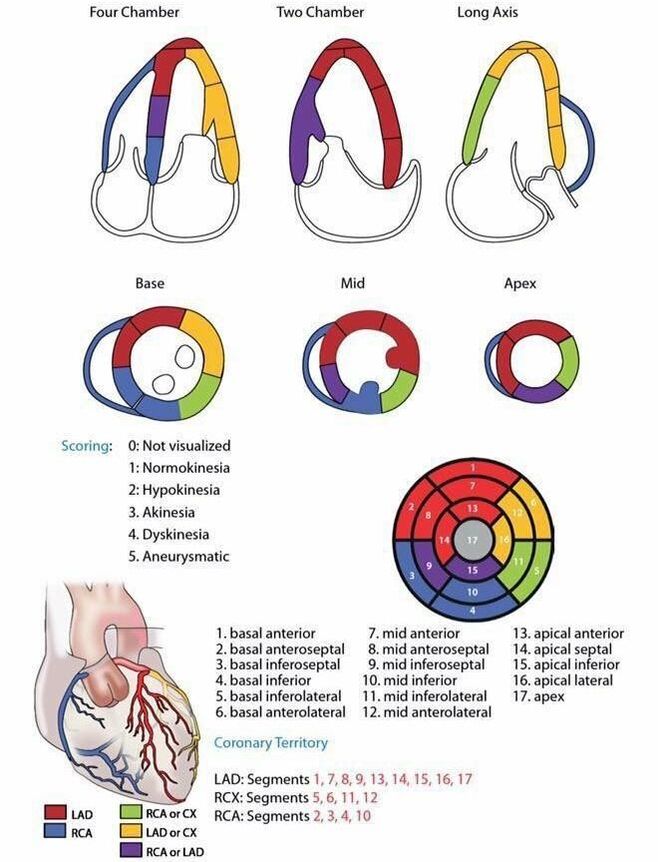
When one portion is not moving in a particular cardiac view, it can be related to a coronary artery. The three main arteries of concern are the left anterior descending (LAD), left circumflex artery (LCx), the the right coronary artery (RCA). Below are two visual concepts of how the coronary arteries are mapped out (creators unknown). Notice the slight variations between the two. Both can be helpful representations of what to look for based on your windows.
The video above is from the Ultrasound Podcast and is meant to be a brief review of the technique. Below it is a GIF from Ben C. Smith @UltrasoundJelly. As with the images above, there are some slight variations which are worth noting when comparing them.
Now that we know the technique and what to look for, what is the evidence? Speckle tracking has been proposed as a more objective way to measure wall motion abnormality. However, a paper published by Reardon et al in 2018 in The American Journal of Emergency Medicine demonstrated that it speckle tracking is not ready for prime time. In the small retrospective study it was not very sensitive or specific for the diagnosis of acute coronary syndrome. If you want a more detailed discussion of this paper check out the Ultrasound GEL Podcast and blog post on this topic.
However, a study published a year later (2019) by Croft et al in the same journal demonstrated that RWMA had a positive likelihood ratio (+LR) of 11.5 and a negative likelihood ratio (-LR) of 0.13 for patients with a myocardial infarction. A secondary outcome was the accuracy of localization for which the +LR was 5.4 and the -LR was 0.13 in this small study of 69 patients. The latter is not too surprising given the variations of the coronary artery mapping as seen above, but overall these are very positive results. The study was done with nine residents (5 PGY1, 3 PGY2, and 1 PGY3) after some short training which helps reflect the ease of application. It is worth noting some limitations of this study with the most important being that this was limited to patients with ST elevation myocardial infarction (STEMI) but is understandable as an investigative study. This would help ensure the high enough incidence rate needed for true positives. However, we are less likely to use this in STEMI patients given the importance of time and ultrasound could delay care. A noteworthy exception is that if the ultrasound is indicated for other reasons such as to evaluate for other important pathology such as an aortic dissection or pericardial effusion. While it is understandable that in theory we could apply this to patients who do not have a STEMI, we need data to support this assumption before we extrapolate too much. Some other limitations to note is that per usual for ultrasound studies this was limited to a single center with a convenience population. There was also a potential for bias since those performing the ultrasound would know these were STEMI patients, but this would not necessarily be different from the real world. It is also worth noting that there was variation in the accuracy of those performing the exams which may demonstrate that this is more dependent skill (more so compared to other exams). What does this mean for RWMA in MIs? While we may not have the strongest evidence to support the routine practice in emergency medicine. It may be another data point when we assess patients that we have concern for acute coronary syndromes. As always, more research is needed to explore the accuracy of RWMA in other populations and to examine for patient oriented outcomes. If you want to learn more about ultrasound, make sure to check outPractical POCUS. A new course just opened which will be in St. Louis, Missouri June 7-9, 2020. This will be a family fun and friendly event at the St. Louis Zoo where students can enjoy themselves and learn how to master their skills. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
2 Comments
Aeraj Peerzade
10/17/2020 09:39:20 pm
good
Reply
Steven
4/2/2024 08:02:29 am
Good
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed