|
Tibial plateau fractures can be easily missed, especially to the untrained eye. Missing these important fractures can have devastating outcomes. In this post we will talk about how to identify and manage these fractures.
Introduction
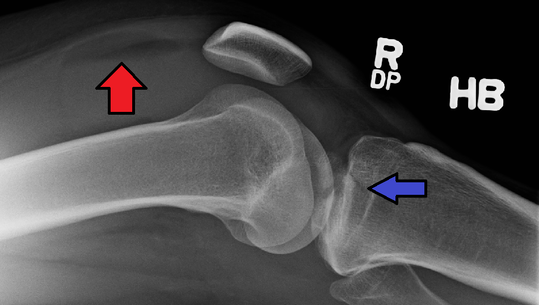
While uncommon, tibial plateau fractures account for approximately 1% of all fractures and are usually seen with high-energy mechanisms such as a motor vehicle collision, fall from significant height, or extreme sports. However, those with osteoporosis can have less severe mechanisms causing these fractures which can make the diagnosis sometimes more challenging. These fractures can cause damage to the nearby vasculature, nerves, ligaments, menisci, and adjacent compartments. Typically, these patients will need some form of surgical management. Anatomy The tibia is the weight-bearing bone of the lower leg and has two articular surfaces at the tibial plateau. The medial tibial condyle bears 60% of the knee's weight and is thicker. The lateral condyle is located slight more proximal than the medial tibial condyle. It is also convex in shape, thinner, and weaker compared to the concave medial tibial condyle. Between the two is the intercondylar eminence and serves as an attachment point for the anterior cruciate ligament (ACL). There are other structures such as the menisci and ligaments of the knee that come into contact with the proximal tibia and can all be injured with these fractures. Compartment syndrome is possible with the anterior, posterior, and deep compartments of the lower leg. The popliteal artery runs posterior to the knee and is the main artery of concern with such fractures. Assessment Given that this often requires severe mechanisms, it is important to assess for other injuries. In addition to the expected knee pain, patients will often have swelling and possibly a deformity. Open fractures can occur and the skin should be closely assessed. The risk of neurovascular injuries prompts close evaluation of sensation, motor function, and distal pulses. Ankle-brachial indices (ABIs) can be used to assess for a difference between extremities. Laxity of more than 10 degrees at the joint line with varus and valgus stress suggests a tear to the collateral ligaments. If the laxity is below the joint line this is indicative of a displaced fracture. Usually, range of motion is difficult to assess due to pain and the patient often will not even to attempt weight-bearing due to pain. Imaging Plain x-rays are the initial study of choice, but their sensitivity is only 79% with lateral plateau fractures and only increases to 85% when adding oblique views. The presence of lipohemarthrosis can be seen in occult fractures (red arrow in the introductory image with blue arrow being the fracture). When there is high suspicion based on mechanism or presentation (such as unable to bear weight or in severe pain), CT should be the next step as MRI is often not feasible in emergency settings. Even when a fracture has been identified, many orthopedic surgeons still prefer having the CT to better evaluate injuries. Below is an example from a BMJ case report in 2017: (A) An anteroposterior projection of left knee demonstrated no evidence of fracture. (B) MRI (coronal T2-weighted fast field echo imaging) revealed left tibial plateau fracture. (C) MRI (coronal proton density-weighted fast spin echo imaging) revealed left tibial plateau fracture.
Management
An often neglected part is pain control. We sometimes may think these patients are exaggerating especially when tibial plateau fractures are not high on our differential. Once identified, a consult with orthopedic surgery is a must for these fractures, even when it is not displaced. The rates of complications are high given the risk for neurovascular injury, compartment syndrome, and infection. In most cases, surgery will be needed with a few exceptions. Infection and other complications such as deep venous thrombosis are concerns after surgery. Even with prophlyactic antibiotics, the infection rate can be over 20%. It is important to know that these injuries will take months to recover. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed