|
One of the most commonly feared diagnoses to miss in medicine is the ruptured aortic aneurysm or aortic dissection. Despite classic teachings, the presentation of most patients is not textbook. While there are many studies trying to find ways to help with the evaluation, they have been limited in success. However, what if you add ultrasound? We discuss some new evidence in this post.
The aorta has always been a challenge. The presentation can be non-specific and imaging has its own challenges. Computed tomography angiography (CTA) exposes patients to both radiation and large doses of intravenous contrast. While it may be necessary to perform, we want to avoid such a test on an undifferentiated population. Transesophageal Echocardiography (TEE) and Magnetic Resonance Angiography (MRA) also present diagnostic challenges as they can be difficult to perform in a timely manner. Some of these patients may not be the most stable to wait for such tests either.
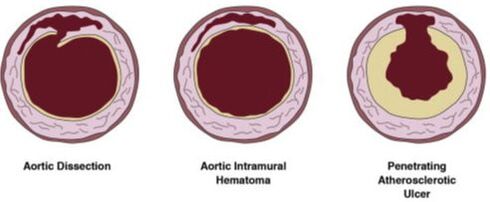
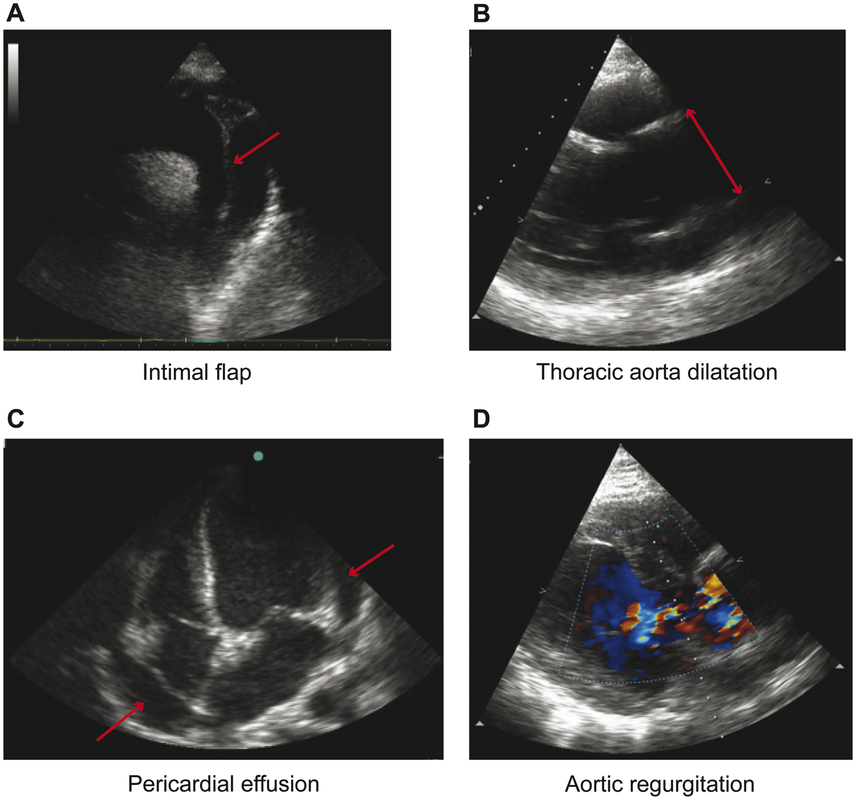
However, Transthoracic Echocardiopgraphy (TTE) can be of potential benefit. You may have heard of focused cardiac ultrasound (FoCUS). There are essentially four key findings you are looking for in regards to acute aortic syndromes (AAS). Indirect signs include thoracic aortic dilation (4cm or greater), aortic regurgitation (on color Doppler), and pericardial effusion (with or without tamponade). The direct signs of a thoracic aortic dissection would be an intimal flap as well as an intramural aortic hematoma (>5mm) or a penetrating aortic ulcer (crater-like outpouching with jagged edges in the aortic wall). Anything that looks like a valve flapping in the aorta is concerning for a dissection. Image A below is looking at the suprasternal notch view. While more challenging to see, a parasternal long axis view or even a parasternal short axis view can be used. Below is an example of the different direct signs for AAS used from another paper.
In regards to abdominal aortic dissections the indirect signs are abdominal aortic aneurysm (AAA) as well as potentially the thoracic indirect signs depending on the extension. Direct signs would be the intimal flap, intraluminal aortic hematoma, and penetrating aortic ulcer just like we would see for a thoracic aortic dissection.
If you want to find some great examples on how to perform the exam as well as some examples, check out 5 Min Sono. Here is the link to the aortic dissection video and here is the link to the examples. The POCUS Atlas also has a lot of great examples here.
Now that you have an idea of how POCUS can play a role, we should go into the new evidence.
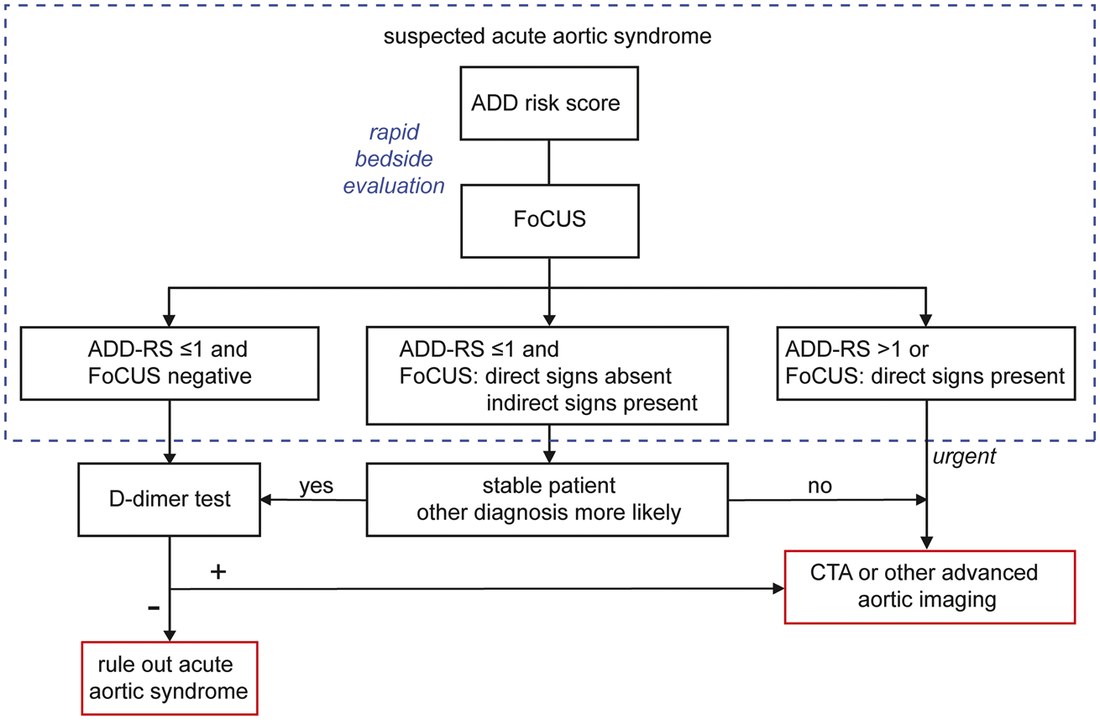
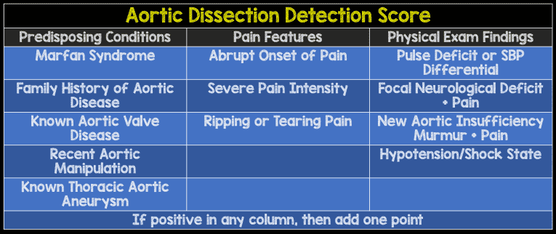
In June 2019, the European Heart Journal published Nazerian et al's paper on using focused cardiac ultrasound (FoCUS) to diagnosed acute aortic syndrome. Research Gate has it free to access and download here. The image above as well as the diagram below are from their paper. With the diagram below, you may be asking yourself how would you know their Aortic Dissection Detection Risk Score (ADD-RS). Fortunately, MDCalc has published the calculation on their website as a reference. If you are having trouble accessing it that way, the table below the diagram, from REBEL EM, can be a useful aid.
Why should we use the evidence? Let us talk first about how they obtained the data. This was from the Aortic Dissection Detection Risk Score Plus D-dimer in Suspected Acute Aortic Dissection (ADvISED) group. That study used the ADD-RS with a D-dimer for risk stratification. They found that the combination of ADD-RS of one or less with a negative D-dimer (defined as <500 ng/mL) as having a sensitivity of 98.8% and a negative likelihood ratio (LR-) of 0.02 which by itself was not bad. However, the paper above was a pre-specified secondary sub-analysis of that study.
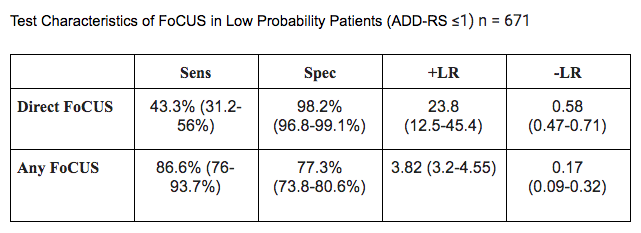
Patients in the study were 18 years or older where AAS was in the differential (it was felt that it needed to be ruled out) where FoCUS was performed prior to advanced imaging or surgery and the patient had at least two of the following: chest/abdominal/back pain, syncope, sign/symptoms of perfusion deficits (nervous system, myocardium, abdominal organs, limbs). They were excluded if trauma was primary or the patient did not consent. The original publication had 1850 patients with 864 patients being eligible and 839 being enrolled in the study. 17.4% of patients had AAS with only 5.2% having direct signs present. How accurate is ADD-RS and FoCUS in combination? The chart below seems to be pretty reasonable. The overall sensitivity is 93.8% with LR- of 0.09 and a failure rate of 1.9% (0.9 - 3.6).
Adding a D-dimer is even more sensitive. A low probability patient by their ADD-RS with no direct FoCUS signs and a negative D-dimer was 100% sensitive (confidence interval 97.3 - 100%), specificity of 58.7 % (confidence interval 55 - 62.4%), and a LR- of 0 (confidence interval 0 - 0.1). If the FoCUS was completely negative this was still 100% sensitive but it brought the specificity down to 48.4%.
What about the positive cases? FoCUS alone with direct signs had a positive likelihood ratio (LR+) of 17.4 and LR- of 0.56 but when you add ADD-RS the LR+ increased to 23.8! This helps demonstrate the accuracy of FoCUS with direct signs. However, any signs on FoCUS were not as helpful. Essentially, when the workup on the algorithm is negative, it is quite safe to discharge based on this study. However, when direct findings are observed on FoCUS we should be very concerned for these patients. As always, validation is needed to confirm what we are seeing in this study. We must remember that this was a secondary endpoint to a prior study so it should be considered more hypothesis generating. It only involved about half of the original population and this is most likely because of the lack of FoCUS being performed in the other patients. Not everyone received further imaging and cases could have been missed on the 14 day follow up. There are also some challenging aspects to the exam. While an intimal flap can be readily identified, an intramural aortic hematoma or especially a penetrating aortic ulcer can be far more challenging. If you want to learn more about the original paper check out The SGEM and First 10 EM. For more reviews on this new paper incorporating FoCUS check REBEL EM and Ultrasound GEL Podcast. Our friends over at Practical POCUS are always happy to teach ultrasound. They offer a variety of courses with their newest course being in St. Louis, Missouri June 7-9, 2020. Make sure to check out this course with emphasis on both adult and pediatric patients. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
2 Comments
Usman Afzal
11/29/2020 03:55:15 am
Informative
Reply
Steven
4/2/2024 08:02:53 am
Interesting
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed