|
Rule out criteria can be our best friends or our worst enemies depending on how we use them. They are not perfect, but can save us from a lot of over-testing. In this blog and podcast, we talk about the good and the bad along with how to use rule out criteria appropriately.
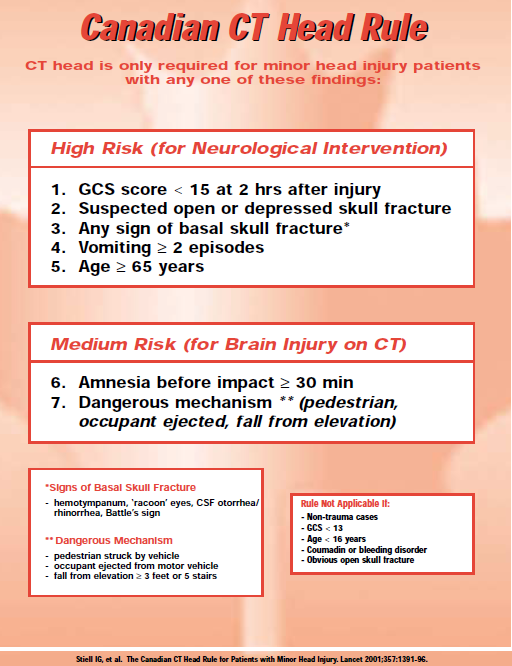
The graphic above on the Canadian CT Head Rule taken from The SGEM demonstrates, there are quite a few criteria that would satisfy the need for a head CT while reducing the need for testing. However, as in the podcast there was the scenario of a 36 year old male who was hit to the temporal area by a softball. He did not satisfy any of these criteria, but given the injury was to the temporal bone area (even though no signs of a fracture), a CT was decided to be performed after thorough discussion of the risks, benefits, and potential complications. When it came back positive for two types of head bleeds (and no fractures as clinically suspected), the patient was then transferred to definitive care. It is worth noting that this does not mean the patient always needs a head CT. The bigger goal is to recognize that rule out criteria are not perfect and that clinical gestalt is key.
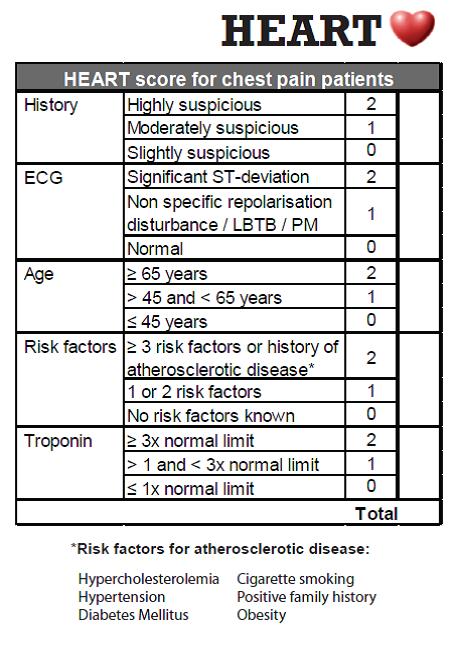
Let us talk about another example, this time with the HEART Score and its graphic found here. A score of 3 or less is considered low-risk and the major adverse cardiac event risk (MACE) is considered to be in general less than 2%. However, a patient with a STEMI but no other findings (troponin not yet elevated or only minimally) and otherwise considered to be low risk (have 3 or less points) is not going to be discharged home with a low MACE risk. Keep in mind, gestalt is what helps you use such a tool to its full potential. It is not meant to replace clinical judgement.
On that point, this podcast is not meant to steer providers away from using such tools. In fact, there are multiple benefits to using such scores. Overall, their accuracy is rather high especially once validated. One of many such examples is from a recent study when providers did an override on the protocol that says a patient did need additional evaluation for a pulmonary embolism (PE) when it was not indicated. Those who did the override were less likely to find a PE than those who kept with the protocol. Another benefit to rule out criteria is that it leads to a point of discussion with patients based on clinicla research. Rule out criteria are essentially never perfect. Even in the rare 100% sensitivity study, that does not mean it will truly capture all cases. Albeit rare, someone is bound to have the disease process. The important part is to think of rule out criteria as risk stratification. Going back to PEs, a generally accepted rule is that 2% is often an acceptable miss rate as evidenced by the PERC Rule. The thought there is that the risk of a workup for a patient suspected of having a PE and the potential over-treatment of a small PE is equivocal at this rate. Hence, we must accept that some patients may be missed. Patients need to know that there will be a potential missed diagnosis. Shared decision making is one of the ways to do this and allows the patient to help make an informed decision. After a proper history and physical, review of the risk stratification tool to be used, and an informed disccusion, both the patient and the provider can come together to make an informed decision. It is important to explain that there is always the possibility of a missed diagnosis, but that it only happens in a select number of patients. Explanation of why this is an acceptable miss rate can also be discussed. Another important point is to make sure to clearly specify warning signs and symptoms that would require immediate return to the department for further evaluation and treatment. Often, these will be the same as what the criteria has outlined. After this discussion, it is important to document this. One tip is to have a template to use that will have the same general outline. Cater this template to each patient as appropriate. Through such a discussion, patients will have a better understanding as to their risks and benefits of testing versus not testing and can make a truly informed decision. Remember, rule out criteria or any other clinical decision aid are risk stratification tools and not perfect. Gestalt and clinical judgement are keys to catching what the tools may miss. Did you like this new approach to a podcast and blog? Do you have any questions? This is our second one and there has been a lot of good feedback. If you are a patient, remember to look at the "For the Public" section for more basic details. Feedback, as always, is appreciated. Remember to look us up on Libsyn, share on Facebook, retweet on Twitter, and rate on iTunes to help spread the word on TOTAL EM. If you have any questions you can comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed