|
We have had many recent firsts on the podcast, and this is the first of two new concepts coming up with a new regular guest, Fritz Fuller. Fritz is a PA practicing in emergency medicine. He plans on coming on regularly for such discussions as these "Tales from the Holler" as well as "Rural Rants" which will be our next type of new podcast. Until next week, enjoy this first episode of "Tales from the Holler."
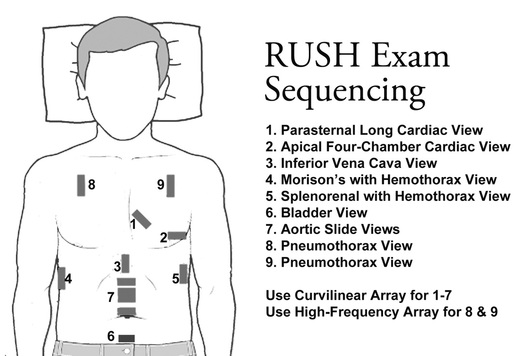
In emergency medicine, we are the experts in managing the undifferentiated sick patient. When it comes to the undifferentiated shock or hypotensive patient, an important for step is the RUSH exam. Above is the RUSH Exam graphic from here and additional RUSH exam information is easily found on EmCrit's website here. RUSH stands for "Rapid Ultrasound for Shock and Hypotension" which is part of Point of Care Ultrasound (POCUS). The original RUSH article can be found here on EmCrit. There are other similar versions that exist such as the "Concentrated Overview of Resuscitative Efforts" (CORE) exam with one such CORE exam article found here. Essentially, think of any of these POCUS approaches for those sick patients who answers are needed quickly, especially when other imaging is either not available or not safe to obtain. Remember, taking a patient to the CT scanner is dangerous especially when they are unstable.
It is important to remember that patients who are hypotensive are in need of resuscitation. In many cases this means intravenous fluids using in the form of crystalloids. However, in the patient with significant and acute blood loss there is the need to replace the lost blood with more blood. Do not rely on labs with acute blood loss to tell you that the patient is low on blood. This needs to be a clinical diagnosis in the unstable patient. Unnecessary crystalloids could potentially harm the patient even more where blood products will be much more beneficial. Asking for help is important to recognize early. We all want to dominate and be the best at every aspect of our field, but quite honestly the field of emergency medicine and especially medicine in general is just too broad. Coworkers probably have their own areas of interest and expertise. There are also those in outlying facilities or specialities who can be of benefit. Know your resources both in house and in outlying centers. When it comes to sick patients, these are some of your best allies. Remember too that it is not just the other providers that can help. All the staff in the department is of use. When locked into a bad situation and no one has the answer, state the uncertainty. Once you mention it out loud, everyone has a chance to bring up their thoughts. Scott Weingart mentions that in his podcast about Stop Points. With such an opening others such as nursing are more willing to assist. Prodcedures such as intubation do not always fix the situation. In fact, sometimes this only makes the situation worse and has a potential to kill the patient. Just like it suggests, the Laryngoscope As a Murder Weapon (LAMW) lecture series focuses on how intubation can kill or signicantly harm a patient. It is a reminder to resuscitate before you intubate as thisLife in the Fastlane article suggests. Measures such as push-dose pressors are also of benefit as mentioned on emDocs and in this Clinical and Experimental Emergency Medicine article. Ultimately, with any procedure weigh the risks and benefits for the patient as it could lead to their demise if not thought through. With sick patients, there is always the risk for fallout. As the late, great John Hinds mentioned there is the risk for Resus Wankers. "Crack the Chest. Get Crucified" is one of the best examples of such fallout. That is not to say that everyone who doubts your abilities is such a person. If you have never listened to it before, consider stopping here to listen to the great SMACC video. However, use colleagues to your benefit and ask for their help. Remember to anticipate for what may happen and become a leader. Those who lead and demonstrate their confidence will be less likely to receive such doubt in the future. A word of caution though is not to do something that is not in the best interest of your patient especially if it is in the hopes of trying to prove something. Finally, communication is key in emergency medicine. One way to do this effectively is sharing a mental model. This Resuscitation Medicine Education (resus.me) post covers many such issues as well as the Chris Hicks SMACC post on "Making Things Work." Planning ahead and preparing can be lifesaving for patients. When possible, discuss plans for time critical situations well in advance. A great time to do that is before the patient even arrives. Do not waste potential down time. Take advantage of those brief periods of freedom to be truly productive. Involve as many people as possible in the development of such plans, especially colleagues who may help manage such a patient. Doing all of this well in advance allows everyone to be on the same page and work more efficiently the day such a scenario happens. Management of critical patients anywhere is difficult. In the resource limited environment of the rural emergency department this can be even more complex. Do you have similar tales? What topics do you want to hear about in the future? Tell us by looking us up on Libsyn, share on Facebook, retweet on Twitter, and rate on iTunes to help spread the word on TOTAL EM. If you have any questions you can comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
2 Comments
Fritz
12/19/2016 08:59:18 pm
Hi Chip, several of your listeners contacts die and asked about the case outcome. My fault for failing to mention it. He underwent continuos renal replacement therapy and eventually fully recovered. It wasn't clear exactly what caused his severe metabolic acidosis but it was likely multifactorial and included some degree of alcoholic ketoacidosis and starvation ketosis. This reminded me of a “newer” nemonic for AG Acidosis- GOLD MARK. Glycols (ethylene and propylene), Oxoproline, L-lactate, D-lactate, Methanol, Aspirin, Renal failure, and Ketoacidosis. (Mehta AN, Emmett JB, Emmett M. GOLD MARK: an anion gap mnemonic for the 21st century. Lancet. 2008;372:892.)
Reply
Chip Lange, PA-C
12/19/2016 09:03:46 pm
Thanks for sharing this Fritz. We also have more people requesting more "Tales from the Holler" and hopefully they will enjoy tomorrow's "Rural Rants" podcast. We plan to have more to come.
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed