|
Summer is often a time that people visit the beach for vacation. While this may be different with the current COVID-19 pandemic, it is still worth learning how to manage one common injury at the beach: jellyfish stings.
It is worth noting that parts of the treatment will vary by species. Recommendations also vary by different organizations usually to reflect local species. It is worth remembering that someone stung by one species may not have the same treatment as someone else in another situation but both still be correct for that patient's injury.
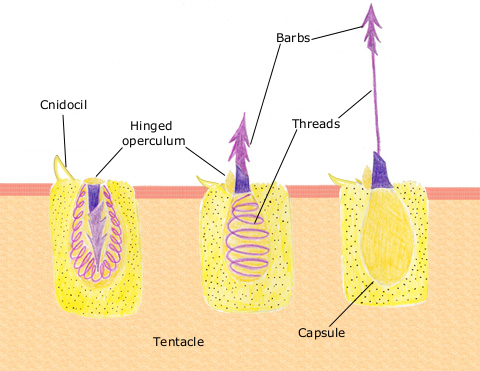
Most of the actual management usually occurs well before the patient arrives at the hospital if they even do come to the hospital. However, it is still worth knowing the spectrum and management as some cases can be severe and even lethal. Nematocysts are used by jellyfish to attack prey and for self-defense. They are spring loaded and deliver the venom that jellyfish carry. Physical contact or an osmotic gradient causes the nematocyst to discharge and release the contained venom. This leads to the well known, stinging pain. However, in some cases it can cause paralysis, cardiovascular collapse, and anaphylaxis.
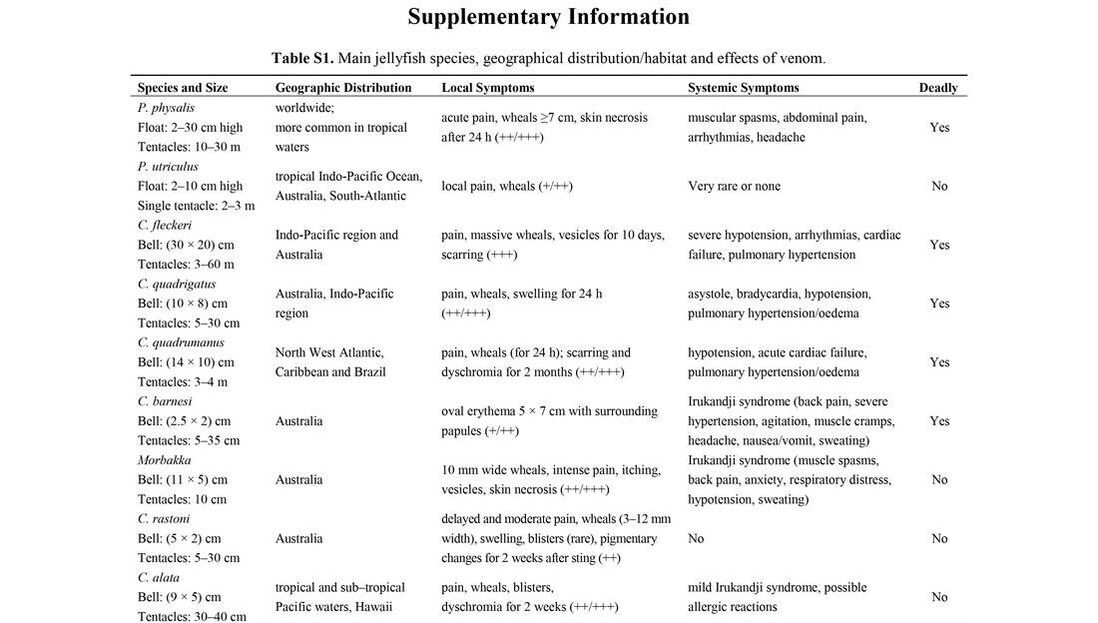
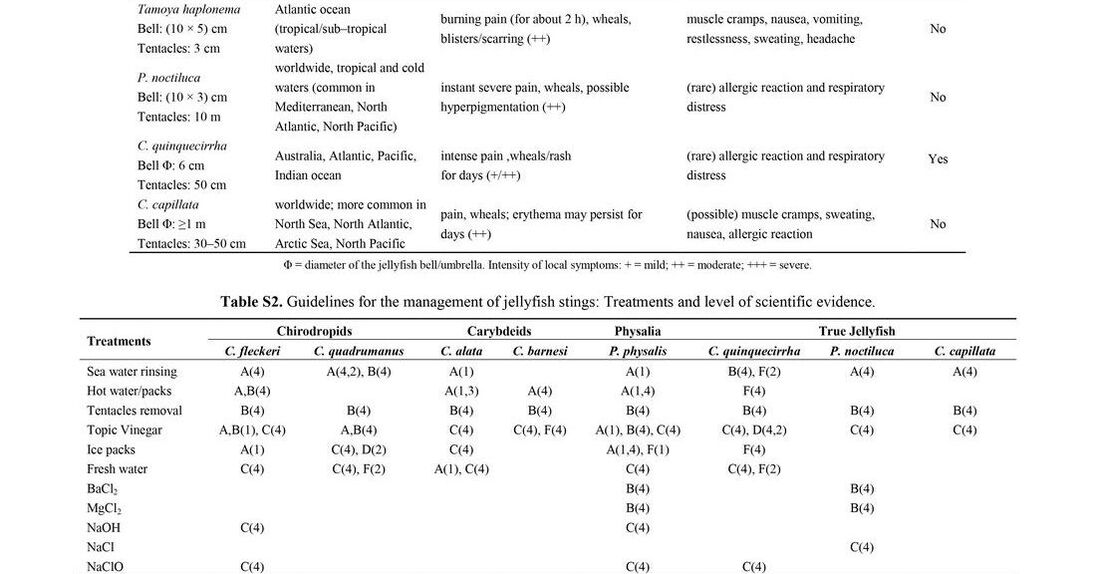
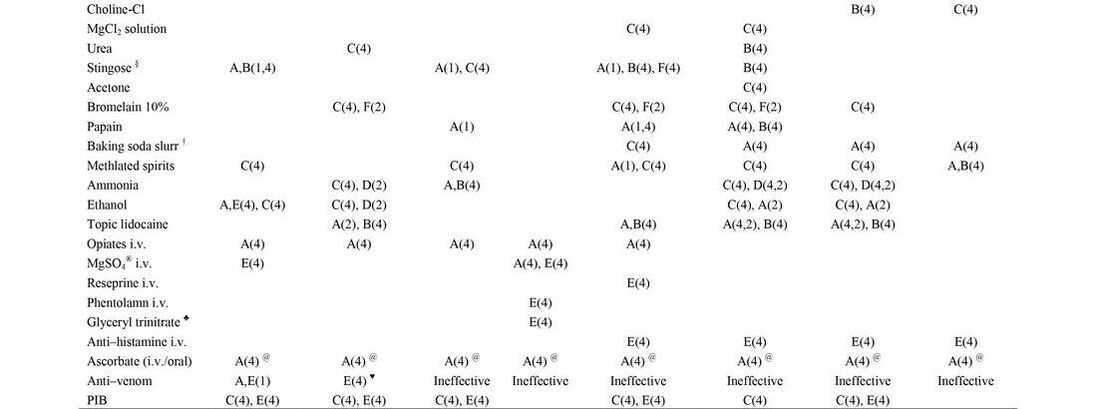
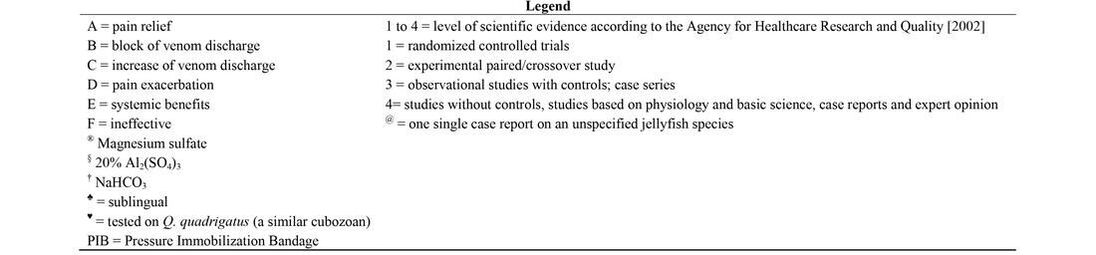
There is an abundance of information on how to treat these injuries and there is a thorough review from the Marine Drugs Journal published in February 2013 by Cegolon et al. that is worth reviewing. If you are looking for a quick reference, check the supplementary information below from that article. It includes a description of the species, its size, where it is located, local and systemic symptoms, if it can be deadly, and various treatment options. If you do not have time to review all of that or want a quick general approach, scroll down some more.
Here is a quick rundown on the key points of management. The very first thing to do is get that person out of the water and keep yourself safe. Some nematocysts can still be present that have not discharged. To help with this, management to deactivate the unfired nematocysts is important. Salt water rinsing is overall quite effective. A slurry created with baking soda is in many cases also effective at stabilizing nematocysts.
Removing tentacles should be performed with a blunt object (sticks, sand castle shovels, etc) and/or thick gloves. It is also important to know that dead jellyfish are not safe as their tentacles can still causing stinging injuries. Avoiding direct contact is important! For pain control and if available the use of hot water packs, topical lidocaine, opioids, and ascorbate (Vitamin C) are all helpful. Hot water packs help denature the toxin (generally at temperatures >43 degrees Celcius). Maintaining this for 20 minutes can provide significant pain relief. Avoid alcohol, urine, and sand as these are not good options. and can actually increase venom discharge and pain. Part of the issue with urine is its close resemblance to freshwater which causes release of venom by altering the salt concentrations. Most other treatments have mixed outcomes. Most patients will not need to go to an emergency department unless they are having a severe reaction. Antivenom is available for Box Jellyfish and some other species. Most of the treatment would be the same in an emergency department as it is in the preshospital setting. Wound care including foreign body removal, wound irrigation, and closure of the wound if needed are all potential components. Updating a patient's tetanus immunization should be considered as well as antibiotic coverage for Vibrio species in grossly contaminated wounds. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on Apple Podcasts. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed