|
Shock, especially in trauma, is an absolute killer. Defined as an abnormality of the circulatory system that results in inadequate organ perfusion and tissue oxygenation, shock must be recognized and treated accordingly. Here to help us with this discussion is Mike Sharma.
The first step of treating shock is to recognize it and then the second step is that it needs to be treated based on the probable cause. Hemorrhage is the MOST COMMON cause of shock in trauma patients!
Any injured patient who is cool to the touch and is tachycardic should be considered to be in shock until proven otherwise. Another helpful tool is to consider their Shock Index which can be easily calculated.
The most effective method of restoring adequate cardiac output, end-organ perfusion, and tissue oxygenation is to restore venous return to normal by locating and stopping the source of bleeding. Volume repletion will allow recovery from the shock state only when the bleeding has stopped.
Definitive control of hemorrhage and restoration of adequate circulating volume are the goals of treating hemorrhagic shock. The presence of shock in a trauma patient warrants the immediate involvement of a surgeon. Strongly consider arranging for early transfer of these patients to a trauma center when they present to hospitals that are not equipped to manage their injuries. The basic principle is to stop the patient's bleeding and replace the volume that has been lost, generally in that order. Persistent infusion of large volumes of fluid and blood in an attempt to achieve a normal blood pressure is not a substitute for definitive control of bleeding.
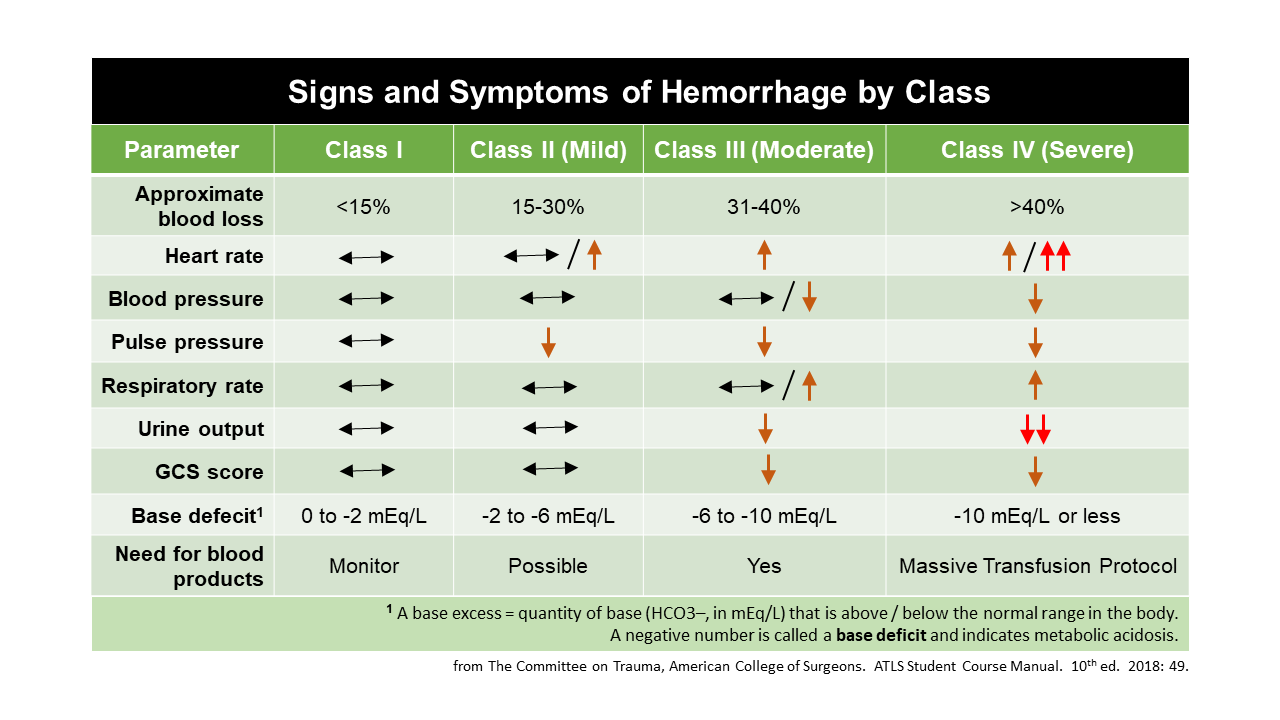
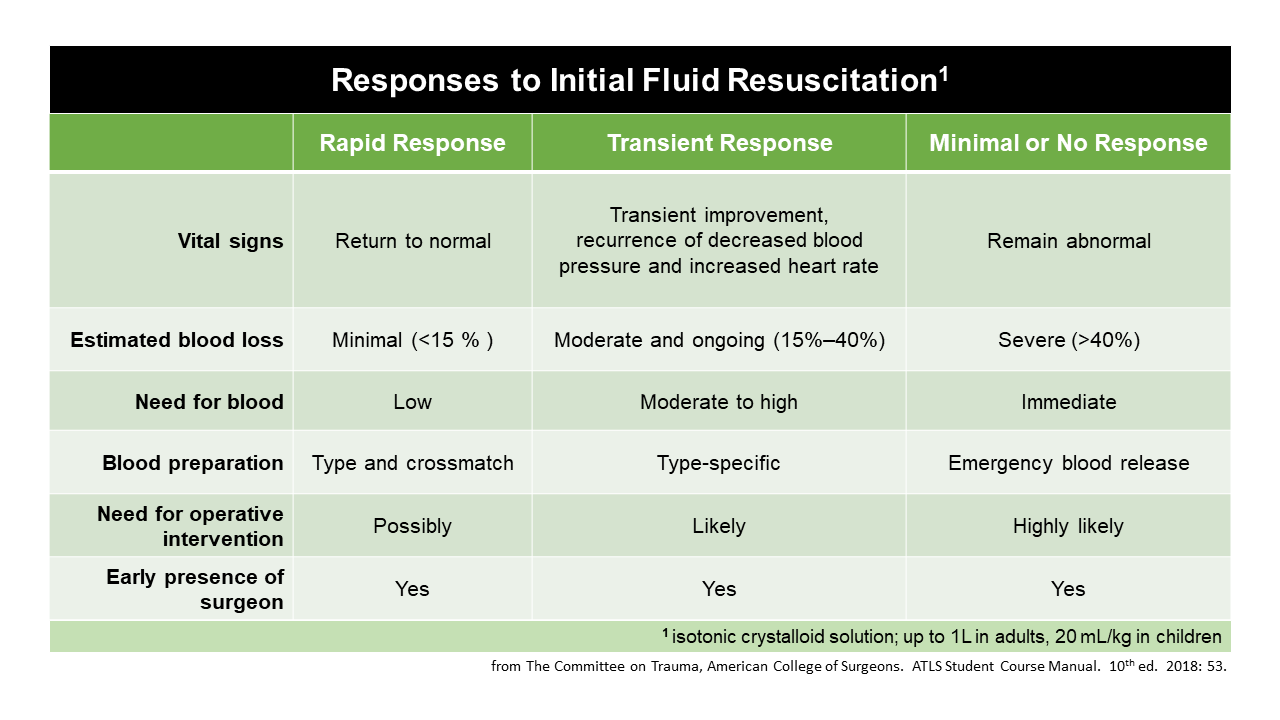
Subsequent volume replacement is determined by the patient’s response to therapy. It is dangerous to wait until a trauma patient fits a precise physiologic classification of shock before initiating appropriate volume restoration. Initiate hemorrhage control and balanced fluid resuscitation begins when early signs and symptoms of blood loss are apparent or suspected—not when the blood pressure is falling or absent.
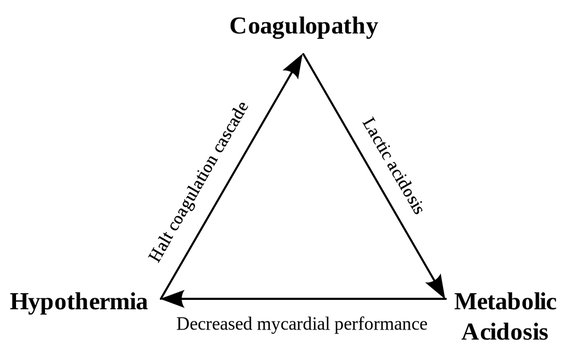
Failure to respond to crystalloid and blood administration in the ED dictates the need for immediate, definitive intervention (i.e., operation or angioembolization) to control exsanguinating hemorrhage. There is a lot of controversy regarding blood versus crystalloids in trauma and if we should use crystalloids at all in trauma. While ATLS recommends a one liter bolus of a crystalloid, it is worth readingthis article to know why that may not be the best strategy. When starting a massive transfusion protocol (MTP) give blood products in a 1:1:1 ratio of packed red blood cells (PRBCs), fresh frozen plasma, and platelets if possible. If readily available, there may be some benefit to giving plasma first compared to PRBCs. Generally, PRBCs will be more readily available though and is usually given first. Consider tranexamic acid (TXA) if the trauma was within the last three hours. An increase in blood pressure should not be equated with a concomitant increase in cardiac output or recovery from shock. DO NOT rely on hemoglobin or hematocrit concentrations, especially early on, to identify blood loss. In cases of massive blood loss, there may be little to no change at the beginning. When exposing a patient, it is essential to prevent hypothermia through methods such as warm blankets being placed as it can exacerbate blood loss by contributing to coagulopathy and worsening acidosis. This leads to the Trauma Triad of Death depicted below.
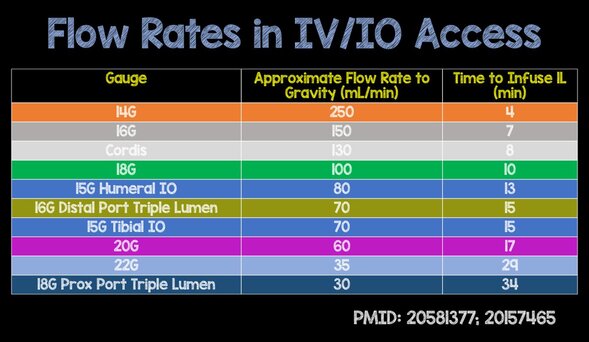
One last important point with shock management. These patients will need medications including blood and/or crystalloids in a rapid fashion. What is the best means of access? While intravascular access is preferred, do not delay treatment by trying multiple times in the unstable patient. Instead, use an intraosseous device which can have rapid infusion rates. Below is a list of flow rates from REBEL EM.
Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on Apple Podcasts. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed