|
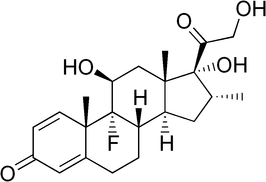
Dexamethasone (the chemical demonstrated here) is commonly used in the treatment of asthma exacerbations both in adults and children. It is growing popularity with new research that supports its role over traditional alternatives such as prednisone. One key difference is its longer lasting effect. However, this new paper demonstrates some potential limitations as discussed in this review.
Title: A Randomized Controlled Noninferiority Trial of Single Dose of Oral Dexamethasone Versus 5 Days of Oral Prednisone in Acute Adult Asthma
Case: A 24 y/o non-pregnant female comes to your department complaining of wheezing and says she used to have an albuterol inhaler but it ran out and she does not have a new prescription. She was treated with two albuterol treatments in the department with significant improvement. You plan to discharge her home with a prescription for an albuterol inhaler and a steroid. In the past she has taken a five day course of prednisone with relief of symptoms, but she says she often forgets to take the pills on the last couple of days and is asking for an alternative, especially one she could take in the department as an alternative. Background: Acute asthma exacerbations account for more than 2.1 million Emergency Department (ED) visits annually and in the US effects 8.4% of the population. Current guidelines from the National Heart, Lung, and Blood Institute recommend a minimum of 5 days of oral prednisone to treat moderate to severe asthma exacerbations (NHLBI Guidelines 2007). Oral and parenteral dexamethasone has similar bioavailability, with the duration of action of 72 hours. Previous studies for pediatric asthma have been promising for dexamethasone as an alternative to other treatments andthere has also been promise with a 2-dose regimen in adults. The thought is that with simple dosing of dexamethasone versus multi-day dosing of routine medications such as prednisone there will be a decrease in the rate of relapse if a single dose medication was used and given in the ED. Clinical Question: Is a single dose of 12mg of oral dexamethasone not inferior to 5 days of oral prednisone in the treatment of adults with mild to moderate asthma exacerbation in preventing relapse? Reference:
Author’s Conclusions: A single dose of oral dexamethasone did not demonstrate noninferiority (meaning it was inferior) to prednisone for 5 days by a very small margin for treatment of adults with mild to moderate asthma exacerbation. Enhanced compliance and convenience may support the use of dexamethasone regardless. Quality Checklist for Randomized Clinical Trials:
Key Results: 173 patients receiving dexamethasone and 203 receiving prednisone completed the study regimen and telephone follow-up. The dexamethasone group by a small margin surpassed the present 8% difference between groups for noninferiority in relapse rates within 14 days (12.1% versus 9.8%; absolute difference of 2.3%; 95% confidence interval -4.1% to 8.6%). Subjects in the 2 groups had similar rates of hospitalization for their relapse visit (dexamethasone 3.4% versus prednisone 2.9%; absolute difference 0.5%; 95% confidence interval -4.1% to 3.1%). Adverse effect rates were generally the same in the 2 groups. Key Points of Debate:
Comparing Conclusions: The study is unfortunately limited due to a number of limitations and the considerable loss of follow-up. This negative study is by no means conclusive but does hold some potential to the applications of dexamethasone in this population. Our Bottom Line: We agree that this study did not demonstrate a single dose of oral dexamethasone to be noninferior to prednisone for 5 days by a very small margin. However, there is still potential for dexamethasone in the treatment of adults with mild to moderate asthma exacerbation. Further studies with fewer limitations and better compliance are needed though to help confirm this hypothesis. Case Resolution: You have a detailed discussion with your patient on the risks and benefits of using dexamethasone versus prednisone. With shared decision making, you discuss how a single dose of dexamethasone may not be enough and that other options such as a two day course of dexamethasone or the five day course of prednisone could be used amongst other options. After careful review, your patient elects to go with the two day option as she feels she can remember to take one more dose at home. After a dose is dispensed here and prescriptions provided, you review your standard return precautions and the patient does well at home. Clinical Application: At this time, the data is very limited in adults for a single dose of dexamethasone. However, two doses of dexamethasone have been shown to be helpful versus five days of prednisone. Until further research can be obtained, alternatives should be considered first before using this option and only after a careful discussion with the patient regarding single-dose dexamethasone. What do I tell my patient? You are having an asthma exacerbation and an important part to treating this is using steroids. We can often give this orally with multiple doses. A new study tried to do a single dose of a steroid known as dexamethasone but was not able to show it was as effective as five days of prednisone. For best effect we can try two days of the dexamethasone of five days of the prednisone. If you feel this will not work we can discuss our options further on the single dose of dexamethasone. Conclusion: Thank you for listening to the podcast and reading the blog. Please let me know if there is anything we need to change or improve. Please remember to help promote us visiting us at Libsyn, sharing on Facebook, retweeting on Twitter, and rating on iTunes to help spread the word on TOTAL EM. If you have any questions you can comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
1 Comment
11/12/2019 08:56:19 am
the facts have been discussed is really important. Thank you so much for sharing a great post.
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed