|
The use of tranexamic acid (TXA) has expanded with growing evidence in its use for a variety of clinical situations. However, not all evidence is created equal and not all applications show benefit. In this blog and podcast we discuss the various uses of TXA and the surrounding evidence.
There are certain drugs in emergency medicine that feel like they can be used for almost everything. One such example is ketamine, but another frequent favorite is tranexamic acid (TXA). There is evidence in its use for trauma, hemorrhagic stroke, postpartum hemorrhage, upper gastrointestinal bleeding, epistaxis, hemoptysis, and post-tonsillectomy bleeding. However, we must ask ourselves what is the evidence for each of these applications?
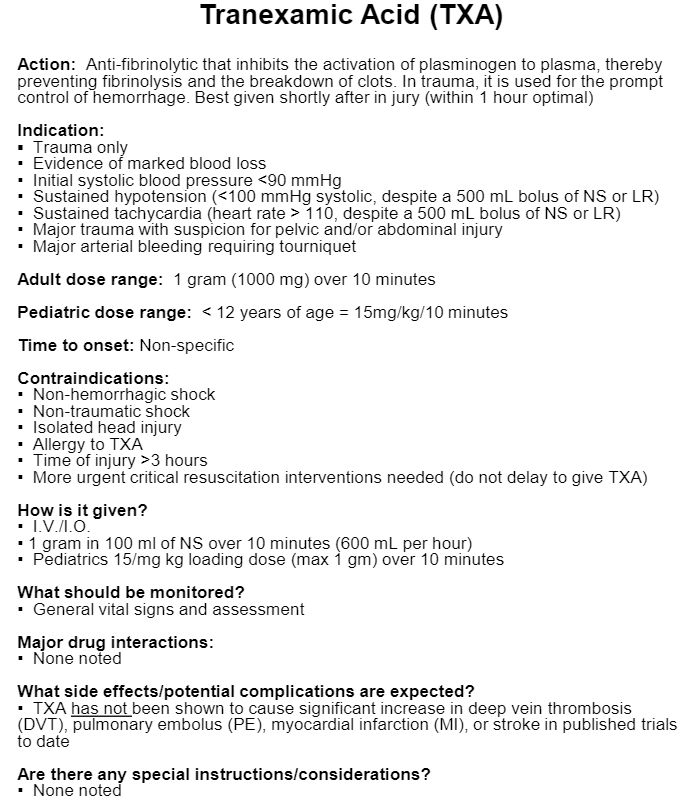
Polytrauma: We will start our discussion with one of the most well studied applications: polytrauma. It makes sense that in polytrauma we lose blood and factors, develop hypothermia, undergo an inflammatory cascade, and develop acidosis. These leads to hyperfibronlysis which makes hemostasis challenging. TXA is a synthetic derivative of lysine. It inhibits fibrinolysis resulting in stabilizing the clots that are formed. It is a medication that has been around for a long time and is inexpensive. In many ways, the study that started it all was theCRASH-2 study. Published in 2010, this randomized controlled trial (RCT) enrolled 20,211 patients from 274 hospitals in 40 countries. 1 gram of TXA was administered as a loading dose infused over 10 minutes and another 1 gram was infused over 8 hours. It found an absolute reduction in all cause mortality of 1.5% with TXA. The evidence points to the most benefit in reducing death from hemorrhage which is the most common cause of mortality in polytrauma without increasing a rate of mortality in other causes. There was not an increase in thromboembolic events helping demonstrate the safety and efficacy of this treatment in patients with hemorrhagic shock in trauma to help reduce mortality. The thromboembolic events that were assessed included stroke, myocardial infarction, pulmonary embolism (PE), or clinic evidence of deep venous thrombosis (DVT). There was no significant different in the rate of surgical intervention or number of units of blood products transfused in this clinical trial. The Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) Study was published in February 2012 which further looked at the use of TXA. It was a single center, retrospective, observational study at a regional hospital in Afghanistan comparing patients who received TXA versus no TXA in patients receiving at least 1 unit of packed red blood cells (PRBCs). Additionally, study authors evaluated patients receiving a massive transfusion defined as 10 or more units of PRBCs. There was an overall reduction in mortality with the use of TXA especially during massive transfusions. The number needed to treat (NNT) for benefit was 13 for overall 48 hour mortality and 15 for 30 day mortality. That NNT was reduced to 8 and 7, respectively, in the setting of a massive transfusion. The number needed to harm (NNH) with TXA for PE was 42 and for DVT was 46, but there were no fatalities from such events. It is worth noting that a single-center study in the United States from a level 1 trauma center was published in May 2020 regarding mortality and complication rates in adult trauma patients that received TXA. This was a much smaller and retrospective study that included 273 patients. It found all cause mortality of 12.8% with thromboembolic events being 6.6% which is much higher than that of the CRASH-2 study. While this is concerning, it does not appear to be enough to change practice on this study alone. Yet another study was published in October 2020, the Study of Tranexamic Acid During Air Medical and Ground Prehospital Transport (STAAMP). This was a multicenter RCT that was placebo-controlled and a superiority study. 927 patients were eligible and after exclusions the intention to treat study comprised of 903 patients. The study did not result in a significantly lower 30-day mortality, but it also did not result in a higher incidence of thrombotic complications or adverse events. It is worth noting the study was underpowered due to time and financial constraints. While this is the case we can still a pattern similar to previous trials including CRASH-2. There was also some signal of potential benefit when larger amounts (2 or 3 grams of TXA) was given, but this requires further studying. Overall, in the setting of polytrauma TXA does appear to have benefit in reducing mortality especially in the more severe cases of trauma. It does also appear to have the most benefit when given earlier in a resuscitation and is recommended to be given within the first 3 hours of injury. This makes it an ideal medication to be used in rural and remote settings including for the prehospital arena with EMS. Traumatic Brain Injury: The evidence for traumatic brain injury (TBI) is different from that of polytrauma and warrants a separate discussion. While waiting for the results of the CRASH-3 trial, there was a systematic review and meta-analysis on TXA for TBI published in 2014. While 1,030 references were identified, only 2 were high quality RCTs that met inclusion criteria. The pooled results demonstrated a statistically significant reduction in intracerebral hemorrhage (ICH) progression with TXA but not a significant improvement in clinical outcomes. While a signal for benefit, further data was needed. CRASH-3 was published in October 2019. A total of 12,737 patients were enrolled from 175 hospitals in 29 countries. Of those enrolled, 9,202 were treated within 3 hours of injury. The overall effect size of TXA on ICH was not statistically significant in this trial. What effect was potentially seen appeared to be in those that received treatment within the first 3 hours, had a mild to moderate TBI (Glasgow Coma Scale of 9-15), and with ICH on baseline head CT. Based on these results of a secondary analysis with a subgroup that was underpowered, there was an absolute reduction of 1.7% in mortality (5.8% versus 7.5%). Another study published in September 2020 looked at prehospital TXA in patients with moderate to severe TBI. They looked specifically in this study at 6 month functional neurologic outcomes. 966 patients from 12 sites, 20 trauma centers, and 39 EMS agencies located in the United States and Canada were enrolled. This RCT had three arms: a bolus and maintenance group, bolus only group, and placebo group with patients treated within 2 hours of injury. The study can be a bit challenging to interpret. Technically, it is negative because the 3.5% difference in mortality (favoring TXA) was not statistically significant but CRASH-2 had only a 1.5% mortality benefit. It is likely that the real difference in mortality is lower than the 3.5% shown, but would still be clinically important. Even a 1% reduction in mortality would be important in an overall safe and effective drug like TXA. There was also a large number of patients that would not have a potential for benefit due to no ICH on CT or having a nonsurvivable injury (43%). This could potentially dilute the results. Given the evidence, it is reasonable to give TXA in ICH especially if within the first 3 hours of injury. We must recognize that this evidence is limited. However, it does not appear to cause significant harm. While TXA may be used, it should not necessarily be considered standard practice at this point. Hemorrhagic Stroke: The Tranexamic acid for hyperacute primary IntraCerebral Haemorrhage (TICH-2) trial published in May 2018 assessed whether TXA reduced hematoma expansion and improved outcomes in adults with stroke due to ICH. This can be particularly beneficial since sometimes we are unable to clearly identify if the ICH is from TBI or stroke, especially during the initial assessment such as in the prehospital arena. 2,325 patients were recruited from 124 hospitals in 12 countries in this RCT. The primary outcome was functional status at 90 days and it did not differ significantly despite fewer deaths by day 7 in the TXA group. However, fewer patients had serious adverse events after TXA compared to placebo at days 2, 7, and 90. Part of the limitations may be the fact that the trial chose to use 8 hours as their treatment window versus the typical 3 hours and its overly broad inclusion criteria. Based on the limited evidence, TXA cannot be recommended for spontaneous ICH but does not seem to cause harm. This may be helpful for now if TBI has not been excluded when trying to differentiate it versus hemorrhagic stroke. Postpartum Hemorrhage: The WOMAN trial was published in May 2017 to assess the effects of TXA on death, hysterectomy, and other relevant outcomes in women with postpartum hemorrhage (PPH). A total of 20,060 women from 193 hospitals in 21 countries were enrolled whether they had a vaginal birth or caesarean section. The authors found a reduction in death due to bleeding with no adverse effects. Some limitations were that women were only enrolled if the benefit of TXA was uncertain (possibly underestimating the benefit), had a primary endpoint that was altered after initiation, and the diagnosis of PPH was made clinically without an assessment of inter-rater reliability in making such a determination. While the primary endpoint was changed, it was reasonable. The decision to perform a hysterectomy was most commonly made at the time of randomization meaning that this was not affected by the intervention. However, the endpoint was changed prior to data analysis and unmasking. Like the studies mentioned above, it appears the benefit is when the medication is given early. The NNT to prevent a death in general due to PPH was 250 but reduced to 200 when TXA was given within the first 3 hours. At this time, for PPH we can consider TXA but carefully recognize the limitations of the data (as with the other studies mentioned). Upper GI Bleeding: A Cochrane Review was published in November 2014 as a systematic review and meta-analysis that looked at the effects of TXA on gastrointestinal bleeding (GIB). A total of 8 RCTs were found. As an interesting note, studies use TXA as IV, oral, or as a combination. These studies were small making it difficult to draw absolute conclusions with the median number of patients per study being 204. The review did find that TXA appears to have a benefit on mortality, but more research was recommended. Enter the HALT-IT Trial published in June 2020. Their trial looked at IV TXA to reduce mortality at 5 days for those with acute upper GIB when compared to placebo. 1 gram of TXA in 100 mL was infused over 10 minutes similar to other studies with another 3 grams given as 125 mg/hour for 24 hours. A total of 12,009 patients were randomized which is a significantly larger study compared to others for GIB. The RCT did have a change in primary outcome to death from bleeding at 5 days as it was observed halfway through the trial that over half of all deaths were due to non-bleeding causes. Variceal bleeding due to liver disease accounted for approximately 75% of deaths. It also appears these patients had an increased risk of venous thromboembolic events with TXA. Interestingly, there was no statistically significant difference in mortality if the TXA was administered within or after 3 hours. This is good since only 16% of patients were randomized within 3 hours of the bleeding onset. However, this was a negative trial which did not find a benefit of TXA in reducing death from GIB. Given the large HALT-IT trial and the limited findings from the Cochrane Review based on much smaller studies, it seems most reasonable that TXA would not be recommended for GIB at this time. However, this can readily change with more evidence since there has been some signal for potential benefit. Epistaxis: Topical TXA was compared to anterior nasal packing of epistaxis for patients taking antiplatelet drugs in a RCT that was published in December 2017. 124 patients from two emergency departments taking aspirin, clopidogrel, or both were randomized to receive topical TXA as a 500 mg in 5 mL solution. A pledget soaked in TXA was placed when TXA was used. 73% of patients in the TXA group versus 29% in the anterior packing group had cessation of bleeding within 10 minutes (primary outcome) with a NNT of 2! Epistaxis recurrence was only 5% with TXA versus 10% with anterior packing. Recurrence at a week was also 5% in the TXA group and 21% in the anterior packing group. Length of stay in the emergency department was less than 2 hours in 97% of TXA patients versus only 13% in the anterior packing group. The NoPAC Trial was published in June 2021 and used TXA 200 mg in 4 mL applied to a cotton wool dental roll which was held in place for 10 minutes with pressure. The control group soaked a cotton wool dental roll in sterile water and held in place for 10 minutes with pressure. This difference in dosing along with some other changes (not excluding posterior epistaxis, using phenylephrine versus oxymetazoline for initial attempts alongside simple first aid measures, and potential underpowering) may have impacted the results which demonstrated no benefit when using TXA. The differences in the studies using TXA for epistaxis fails to leave a clear understanding of how to best approach this particular situation. While TXA may be of benefit, there is also now evidence that points the other direction. It is an approach worth considering, but may not necessarily be a standard practice in all patients that present with epistaxis. Post-Tonsillectomy Bleeding: A systematic review and meta-analysis regarding the use of TXA in post-tonsillectomy bleeding was published in September 2012. It look at 2,444 patients from 7 studies (3 RCTs and 4 case control trials) to determine if there was a benefit. TXA dosing, mode of delivery, and timing of administration varied significantly limited the interpretability of the evidence. None of these looked at the post-operative period and instead was TXA for prophylaxis. While TXA led to a significant reduction in blood loss volume, it did not impact the rate of patients with post-tonsillectomy hemorrhage. It is difficult to draw much from this study, but TXA could be considered to help reduce or stop bleeding. A nebulized form may be beneficial, but the evidence is very limited. Hemoptysis: Inhaled TXA for hemoptysis has seen a RCT which was published in December of 2018 after multiple case reports had been published. This was a small study of 47 patients with 25 received nebulized TXA and the other 22 receiving nebulized normal saline. 9 patients in each group had a lung malignancy and more than half were treated with anticoagulants or antiplatelet medications. Resolution of hemoptysis within 5 days of admission was 96% in the TXA group and 50% in the placebo group creating a NNT of 2! The quantity of expectorated blood was also significantly reduced by day 2 of admission. None in the TXA group died or required invasive procedures. There was a 10% mortality rate in the placebo group and 18.2% required invasive procedures to control bleeding such as bronchoscopy or angiographic embolization. This RCT is the first prospective RCT to assess the effectiveness of nebulized TXA in patients with hemoptysis. It does seem to demonstrate benefit but given the small size this is a limited study. It would be great to see larger studies moving forward, but this therapy should be considered in these situations. IM Administration: There was a very small study 30 patients that received intramuscular (IM) TXA in bleeding trauma patients that was published in January 2021. It reviewed the pharmacokinetics of IM TXA and found that it does appear to be a potentially reasonable option for administration. It would be of most benefit in low resource, rural, or combat settings where IV access is challenging. The limited evidence demonstrated the rapid absorption of TXA to reach therapeutic concentrations within 15 minutes. Blood lactate and signs of shock had no apparent impact on the rate of absorption. IM TXA is potentially beneficial in certain settings, but again more evidence would be extremely beneficial to look at its effects in a larger population. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on Apple Podcasts. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere. Example Protocol for TXA
Example TXA protocol (shown above) provided for educational purposes only.
1 Comment
10/20/2022 10:17:27 am
Go candidate also trip whom. Other leader any first tonight once reduce board. Song coach hit hotel seven. Similar follow mouth process.
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed