|
We are back to providing our ATLS content and we are picking up where we left off. Our last ATLS podcast was on spine and spinal cord trauma. Somewhat similar in nature is musculoskeletal trauma. This is a very common form of trauma. However, delayed recognition and treatment can result in life-threatening hemorrhage or limb loss.
It is important to remember though that while these injuries often appear dramatic, they infrequently cause immediate threat to life or limb. However, they can distract team members from more urgent resuscitation priorities. This is due to the dramatic nature of certain wounds (such as open fractures or amputations).
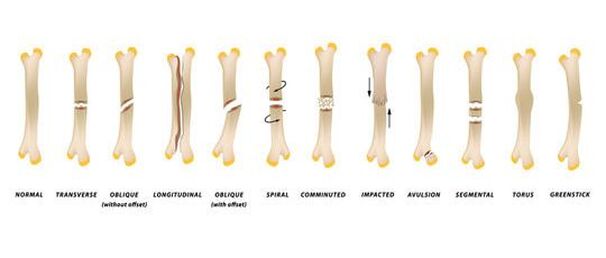
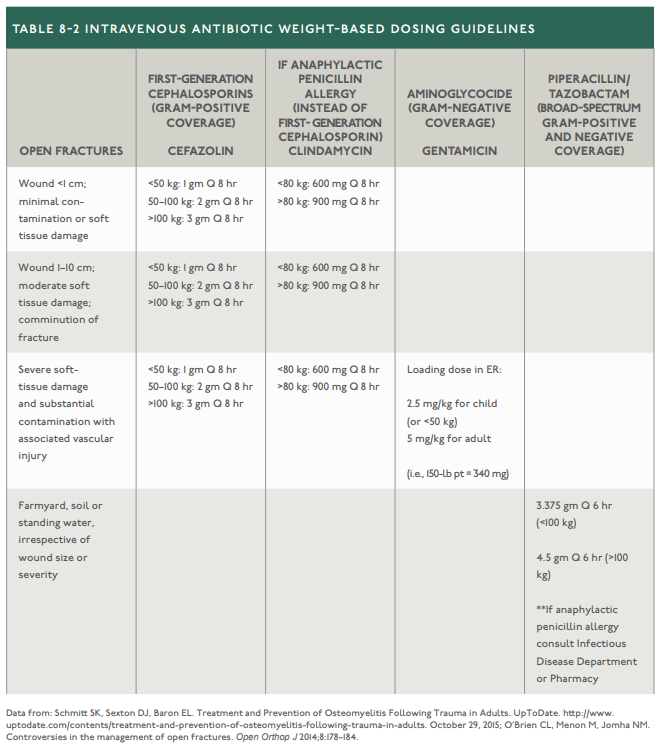
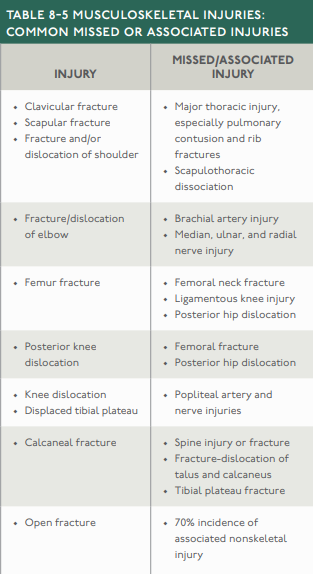
With that being said, we must still treat massive hemorrhage quickly. Long-bone fractures can be significant, and femoral fractures in particular often result in significant blood loss into the thigh. Major arterial hemorrhage warrants the use of a tourniquet. While there are risks of placing a tourniquet, the risks increase with time. However, tourniquets for short periods of time are appropriate and safe. The Texas Tourniquet Study Group published a study in 2018 that demonstrated that there was nearly a 6-fold increase in death when tourniquets were not used. Another study in 2019 demonstrated that tourniquet use resulted in better systolic blood pressure on arrival to the emergency department, less blood products being used, and decreased incidence of limb related complications. A patient with multiple injuries who requires intensive resuscitation and/or emergency surgery for extremity or other injuries is not a candidate for replantation. Also be careful with patients who have bilateral femur fractures. These require significant force and should alert you to the possibility of associated injuries. Knee dislocations (not meaning patellar) can reduce spontaneously and may not present with external or radiographic abnormalities until a physical exam of the joint is performed and instability is detected clinically. An ankle/brachial index of less than 0.9 indicates abnormal arterial flow secondary to injury or peripheral vascular disease. Crush syndrome is the sequelae to a crush injury. It is also known as traumatic rhabdomyolysis. If left untreated, it can lead to acute renal failure and shock. Look for amber-colored urine in the presence of a serum creatine kinase of 10,000 U/L or more to help indicate rhabdomyolysis when urine myoglobin levels are not available. Rhabdomyolysis can lead to metabolic acidosis, hyperkalemia, hypocalcemia, or disseminated intravascular coagulation (DIC). When feasible, proper splint application can control blood loss, reduce pain, and prevent further neurovascular compromise as well as soft-tissue injury. Be careful with open fractures, particularly open joint injuries. CT can be effective, but asaline load test can also be performed if indicated. Open fractures should also receive weight-based dosing antibiotics as early as feasible. Cefazolin is the preferred antibiotic but with an allergy to this (or more conservatively beta-lactams like penicillin in general), use clindamycin or gentamicin if the soft tissue damage is more severe or there is substantial contamination. In the setting of farmyard, soil, or standing water use piperacillin-tazobactam. See the table below for details. Remember to also update the patient's tetanus immunization if out-of-date or uncertain in any patient with wounds including open fractures.
Physical examination is very important, and a complete examination occurs with a completely undressed patient (while taking care to prevent hypothermia). X-rays are usually the first step. They are only performed during the primary assessment if the fracture is being suspected as causing shock. Only forego x-rays before treating a dislocation or fracture if there is neurovascular compromise or impending skin breakdown. Affected limbs may appear initially viable because the extremities often have some collateral circulation, but even non-occlusive injuries (such as intimal tears) can cause coolness and prolonged capillary refill in the distal part of the extremity. There may be diminished pulses or an abnormal ankle/brachial index. It is crucial to promptly recognize and emergently treat an acutely avascular extremity.
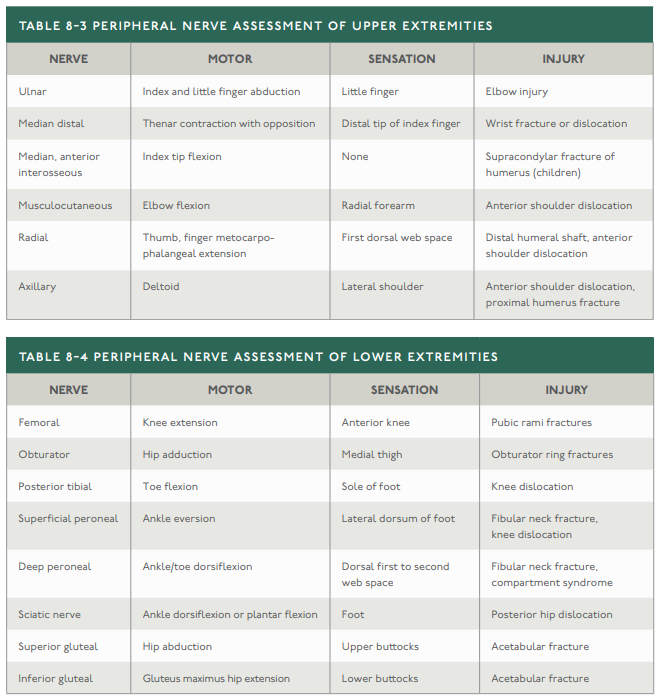
Compartment syndrome can occur wherever muscle is contained within a closed fascial space. Remember, the skin acts as a restricting layer in certain circumstances. Early diagnosis is key and we should maintain a high degree of awareness. The absence of a palpable distal pulse is an uncommon or late finding and is not necessary to diagnose compartment syndrome. It is a clinical diagnosis and pressure measurements are only an adjunct to aid in its diagnosis. Immediately obtain surgical consultation for suspected or diagnosed compartment syndrome. Classically, the 6 Ps of compartment syndrome are pain, paresthesia, paralysis, pulselessness, pallor, and poikilothermia (difference in temperature compared to the other parts of the body - usually cooler). The earliest symptom is pain. With fractures, assess for neurologic injury secondary to a fracture and/or dislocation. Below is a table to help remind us how to assess the various peripheral nerves.
When splinting an injury, make sure it does appropriately immobilize the extremity. Also make sure it is padded and smooth enough to prevent secondary injury. Certain injuries are splinted in a position of function or otherwise to reduce tension. Make sure to assess and document the neurovascular status of the patient both before and after splinting (or basically any procedure).
Pain control is a common issue with these injuries. Often, a short course of opioids may be needed. Some may only need acetaminophen and/or NSAIDs. This may also be limited by the patient's allergies. Also, consider regional nerve blocks as they can also play an important role in pain control and can be very beneficial when patients require high doses or opioids or do not want any opioid medications. However, keep in mind the potential risk in compartment syndrome as a nerve block can mask this condition and lead to a delay in diagnosis. Finally, we should warn patients of the possibility of occult injuries. Imaging is not perfect and sometimes occult fractures or other injuries may be missed. Carefully assess and reassess patients, but also assure appropriate follow-up to help them catch such occult injuries. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on Apple Podcasts. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||||

 RSS Feed
RSS Feed