|
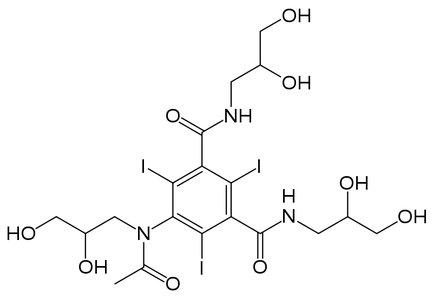
Contrast has been hotly debated in the radiology and emergency medicine world. Many of these contrast medications (such as Iohexol above) have demonstrated safety and efficacy. However, a deep dive has been sorely needed on this subject and with recent relevant papers over the last year this felt like the right time. Joined by Dr. Paul Schunk, we explore the mysteries and evidence that exists for contrast safety in CTs for acute kidney injury and contrast induced nephropathy.
When understanding contrast and its safety, the first step is to define what we are looking for in the first place. Probably the single best source for a definition comes from the American College or Radiology's Manual on Contrast Media version 10.2 with the Post-Contrast Acute Kidney Injury and Contrast-Induced Nephropathy in Adults last updated on November 19, 2014 for the relevant section.
They define post-contrast acute kidney injury (PC-AKI) as "a general term used to describe a sudden deterioration in renal function that occurs within 48 hours following the intravascular administration of iodinated contrast medium. PC-AKI may occur regardless of whether the contrast medium was the cause of deterioration." This means that this is a correlative diagnosis and does not mean the contrast caused the AKI! Now let us take the more difficult to identify contrast-induced nephropathy (CIN) which they define as "a specific used to describe a sudden deterioration in renal function that is caused by the intravascular administration of iodinated contrast medium." That would make CIN a subgroup of PC-AKI but that this is a causative diagnosis. This is harder to actually prove though and is becoming part of a much larger debate including of its very existence. Some other points worth mentioning from the ACR manual includes that they acknowledge CIN being a rare entity and that serum creatinine can be considerably influence by the patient's gender, muscle mass, nutritional status, and age. They instead recommend other measures such as estimated glomerular filtration rate (eGFR) for predicting the true GFR. It is very much worth noting two of the recommendations from the ACR manual that we will discuss more below. The first point is that if the GFR is 45 or greater there is no independent nephrotoxic risk factor and that in patients with an eGFR between 30-44, IV iodinated contrast media is either not nephrotoxic or rarely so. Second, there is little to suggest that contrast is an independent risk factor for AKI in patients with an eGFR at least 30. They are quick to point out though that any threshold put into practice should b weighed on an individual patient level with the risks and benefits compared. Also, when discussing the morbidity and mortality of PC-AKI it is unusual for patients to develop permanent renal dysfunction. A final point before we move on is that volume expansion is the major preventative action in mitigating the risk of CIN both before and after contrast medium administration. The first McDonald paper to discuss is the April 2013 publication with the Radiological Society of North America (RSNA) journal called Frequency of Acute Kidney Injury Following Intravenous Contrast Medium Administration: A Systematic Review and Meta-Analysis. As with any of these papers, a full review is very much worth the time but the key finding to be aware of from this paper was the fact that "controlled contrast medium-induced nephropathy studies demonstrate a similar incidence of AKI, dialysis, and death between the contrast medium group and the control group. There were two somewhat peculiar studies included in the analysis that we explain better in the podcast why they may not have been such good papers and were definitely the odd ones out. McDonald's second paper we will discuss is from the April 2014 issue of RSNA called Risk of Intravenous Contrast Material-mediated Acute Kidney Injury: A Propensity Score-matched Study Stratified by Baseline-estimated Glomerular Filtration Rate. This study had a very unique finding because although the incidence of AKI significantly increased with decreasing baseline eGFR (P < 0.0001) the incidence was not significantly different between contrast material and non-contrast material groups in any eGFR subgroup which was a rather significant and influential finding that most readers were probably not suspecting. The authors go on to talk about how equations to calculate eGFR demonstrated superior correlation to the actual GFR compared to serum creatinine. In 2013 Davenport and his team also published important papers in RSNA with the October 2013 paper called Contrast Medium-induced Nephrotoxicity Risk Assessment in Adult Inpatients: A Comparison of Serum Creatinine Level- and Estimated Glomerular Filtration Rate-based Screening Methods. This more conservative but still influential and pertinent paper found that using an eGFR screening of less than 45 would significantly increase the number of inpatients identified to be at risk for CIN but would help reduce misidentifying those patients who would be considered low risk. If your hospital is currently using serum creatinine for its screening, there is a useful section comparing those cutoffs versus eGFR cutoffs to find what would be most applicable and acceptable at your facility. The September 2013 Davenport paper in RSNA was titled Contrast Material-induced Nephrotoxicity and Intravenous Low-Osmolality Iodinated Contrast Material: Risk Stratification by Using Estimated Glomerular Filtration Rate. This paper discussed how patients with a stable eGFR less than 30 have a risk of nephrotoxicity with low-osmolality iodinated contrast material (LOCM) with a trend toward the same if the eGFR was 30-44. However, if the eGFR was 45 or more prior to CT then LOCM does not appear to be a nephrotoxic risk factor. Again, this paper was more conservative than McDonald's team in their findings but new papers were sure to come. Fast forward to the Journal of the American Society of Nephrology and a paper that was published there by Wilhelm-Leen and her team called Estimating the Risk of Radiocontrast-Associated Nephropathy that was published in September of 2016. In their study the find the risk of AKI appeared to be overstated in the literature and overestimated by clinicians. They mention that in their patients those who received radiocontrast were generally sicker than those that did not receive contrast. This is an important point with regards to certain counterarguments brought up about patients who received contrast and maybe not being as sick. The final paper reviewed today and on the podcast is a paper with the lead author of Hinson published to the Annals of Emergency Medicine titled Risk of Acute Kidney Injury After Intravenous Contrast Media Administration. Its very important confirmed what previous papers such as the ones above suggested in that intravenous contrast was not associated with an increased risk of AKI. This paper is well worth the read but one of the key aspects worth noting in this paper was that there were three groups compared: one where patients received IV contrast with their CT, another where they did not get contrast with their CT, and then the last group had no CT at all. Although not statistically significant, it is worth noting that in each case those who got IV contrast were at the lowest incidence of any of the measured outcomes listed for the study in the paper specifically. Outcomes were also measured long term at six months including very important patient oriented outcomes such as newly diagnosed chronic kidney disease, dialysis, and renal transplant. There was a lot to discuss in this paper along with the others so make sure to listen to the podcast for the other details not mentioned here. This was a long deep dive but there is still plenty of information out there to explore. It is important to review the papers in detail to find the finer points that cannot be discussed fully here. Let us know what you thinks about the papers and the evidence out there by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed