|
We have talked about abscess management before both here (Podcast #13) and on the Skeptics' Guide to Emergency Medicine (Podcasts #156 and #164). Even though we have talked about using antibiotics before, there has been debate on its use in smaller abscesses. Today, we cover how antibiotics are still beneficial even for the small ones given the most recent evidence out there. Listen to podcast and read this blog for all the details as we cover different points in each.
Title:
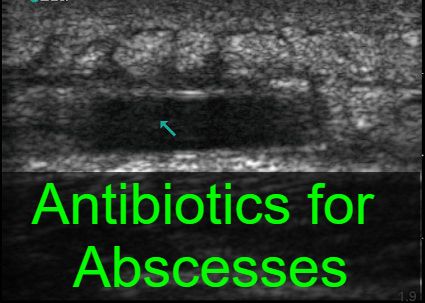
A Placebo-Controlled Trial of Antibiotics for Smaller Skin Abscesses Case: A 34 y/o male with no past significant medical history presents complaining of a skin abscess that has been present for two days. He is afebrile and denies any known drug allergies. On exam you note a 4cm diameter area of erythema and swelling that is warm to the touch. Ultrasound confirms this to be an abscess (similar to the image above from Mount Sinai EM Ultrasound's page). After incision and drainage, you are trying to decide if this patient needs antibiotics. You know the two most common are clindamycin and trimethoprim-sulfamethoxazole (TMP-SMX). However, you do not know if either is needed or which one may be better. Background: Skin abscess are a common complaint across healthcare and a frequent presentation to emergency departments across the world. Staph infections are the most common cause for these infections. Clindamycin and TMP-SMX are frequently used given their low cost along with their safety and efficacy. A recent trial by Talan et al found TMP-SMX in larger abscesses had a higher cure rate than incision and drainage alone. Other studies have done the same for larger abscesses both with clindamycin and TMP-SMX with similar findings for both but did not include a placebo or smaller sized abscesses. Clinical Question: Does clindamycin or TMP-SMX in conjunction with incision and drainage improve short-term outcomes in patients with a simple abscess compared with incision and drainage alone? Reference:
Author’s Conclusions: As compared with incision and drainage alone, clindamycin or TMP-SMX in conjunction with incision and drainage improves short-term outcomes of patients who have a simple abscess. The benefit must be weighed against the known side-effect profile of these antimicrobials. Quality Checklist for Randomized Clinical Trials:
Key Results: A total 786 patients were randomized with 505 being adults and 281 being children. 266 patients were assigned to receive clindamycin, 263 to receive TMP-SMX, and 257 received a placebo. Using the intention-to-treat population, the cure rate at 10 days was 221 in the clindamycin group (83.1%), 215 in the TMP-SMX group (81.7%), and 177 in the placebo group (68.9%) with a significant difference between antibiotics versus placebo (P<0.001). Key Points of Debate:
Comparing Conclusions: We agree that antibiotics (specifically clindamycin or TMP-SMX) improve short-term outcomes in patients with a simple small abscess that has undergone incision and drainage versus having an incision and drainage alone. Our Bottom Line: Even for small abscesses, antibiotics can be beneficial for the treatment of abscesses with incision and drainage especially in cases of Staphlycoccus aureus infections. Case Resolution: After completing the incision and drainage, you discuss with the patient the risks, benefits, and potential complications of antibiotics. With shared decision making, he agrees to antibiotics and you prescribe him medications before he is discharged. Clinical Application: Antibiotics are becoming more frequently used for the treatment of abscesses after incision and drainage. This study further supports the growing use of antibiotics whether for small or large abscesses. However, given its low NNT especially in Staphlycoccus aureus infections, this is a beneficial treatment overall. It is worth remembering that antibiotics are not without risks and should be carefully considered. What do I tell my patient? Antibiotics have been shown to be helpful in treating abscesses in addition to opening up the abscess through an incision and drainage, especially in the staph type infections we often see. These are usually well tolerated but there are some risks such as allergic reactions but it is more often mild symptoms such as nausea and diarrhea. Conclusion: Thank you for listening to the podcast and reading the blog. Please let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until next time, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed