|
After our talk with Minh Le Cong from the PHARM podcast, we decided it was appropriate to discuss the POKER Trial. No, it is not about cards, but rather about if propofol mixed with ketamine is better than propofol alone.
In addition to this podcast, there have been a few other blogs such as St. Emlyn's and REBEL EM that reviewed this study. At this time, we believe that this is the only podcast to create an audio discussion in detail on the subject (we may have missed someone and we apologize). For that reason, we wanted to make sure there was a way you could listen to a detailed analysis of this study soon as it is still a relatively recent publication.
Title: Propofol or Ketofol for Procedural Sedation and Analgesia in Emergency Medicine – The POKER Study: A Randomized Double-Blind Clinical Trial
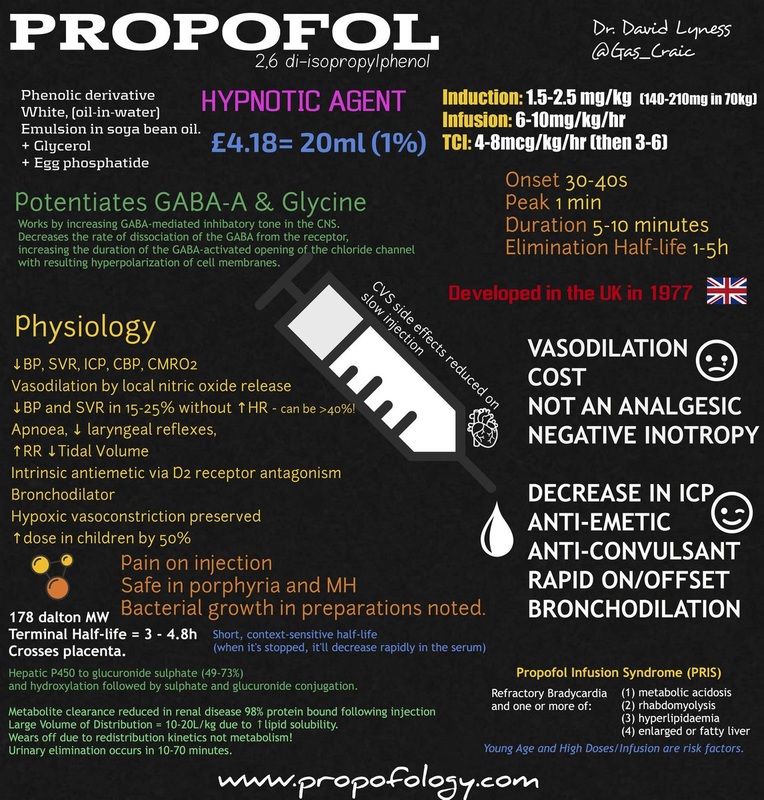
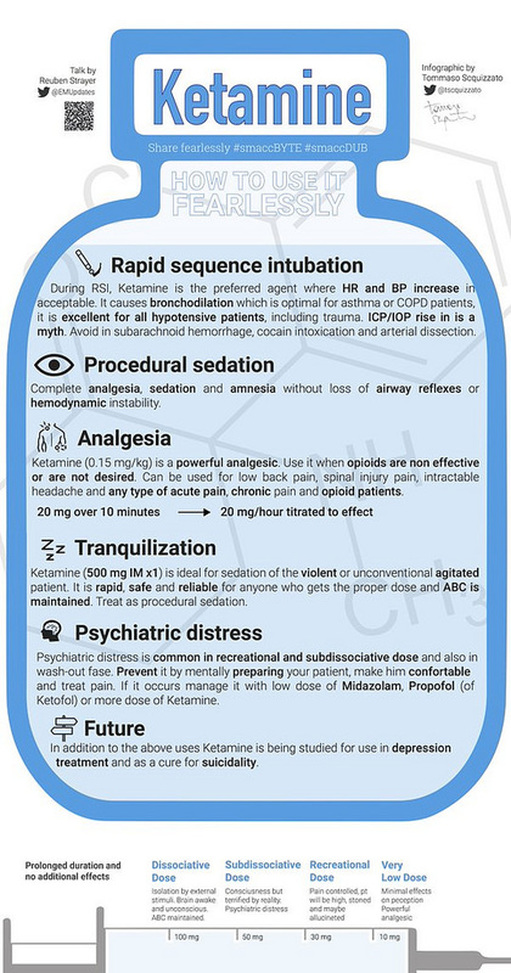
Case: A 32 y/o otherwise healthy non-pregnant female comes to your ED for a shoulder dislocation. A medical student initially assesses the patient and plans for procedural sedation to perform the reduction of the patient’s left dislocated shoulder. While preparing for the procedural sedation, the student asks about using propofol or the new idea of combining ketamine with propofol in a 1:1 ratio. The student wants to know if one of these will be better than the other given the ketofol has theoretical benefits versus propofol alone. Background: Procedural sedation is common in the ED and requires certain medications such as ketamine or propofol. Each medication has its own benefits and risks. Common issues with ketamine are hypertension, tachycardia, vomiting, laryngospasm, and emergence delirium. Propofol has been associated with such complications as hypotension, loss of airway reflexes, hypoventilation, apnea, and hypoxia. There has been an antiemetic effect found with propofol and ketamine helps maintain airway reflexes as well as provide analgesia. There has been a hypothesis that the two medications combined may lead to fewer adverse events compared to propofol alone given that they will “balance” each other out. However, previous single-center randomized controlled trial have not demonstration such a reduction in respiratory adverse events. Clinical Question: Does ketofol in a 1:1 ratio lead to further adverse respiratory events requiring intervention by the sedating physician compared to propofol alone? Reference:
Author’s Conclusions: Ketofol and propofol resulted in a similar incidence of adverse respiratory events requiring the intervention of the sedating physician. Although propofol resulted in more hypotension, the clinical relevance of this is questionable, and both agents were associated with high levels of patient satisfaction. Quality Checklist for Randomized Clinical Trials:
Key Results: There were 591 patients were 296 in the propofol group and 295 in the ketofol group. 4 patients in the propofol group and 14 in the ketofol group did not get sedation after being randomized. This meant there were 573 patients total with 292 receiving propofol and 281 getting ketofol. 5% of the propofol group and 3% of the ketofol group had an adverse respiratory event (the primary outcome) with an absolute difference of 2% (95% confidence interval [CI] of -2% to 5%). Patients receiving proprofol were more likely to become hypotensive (8% versus 1%; difference 7%; 95% CI 4% to 10%). Patient satisfaction was very high in both groups (10/10; interquartile range 10 to 10/10). Although the ketofol group was more likely to experience severe emergence delirium (5% versus 2%; difference 3%; 95% CI 0.4% to 6%) they did have lower pain scores at 30 minutes post-procedure. Key Points of Debate:
Comparing Conclusions: We agree with the conclusion that patients receiving ketofol and propofol had a similar incidence of adverse respiratory events requiring intervention. Although there were lower rates of all events in the ketofol group, it was not statistically significant. Also, the hypotension was most likely not clinically significant, but should serve as a reminder that this does occur with propofol. Our Bottom Line: At this time it does not appear that ketofol has a benefit in decreasing adverse respiratory events when compared to propofol alone. However, there may be other benefits such as adding ketamine to provide analgesia or reducing potential complications with ketamine such as emergence reaction when adding propofol. One must use caution though given the limited evidence of benefit and potential risk of complication when adding two medications together. Case Resolution: You discuss with both your student and the patient the plan for treatment along with the patient’s options. Everyone agrees to try propofol and giving an opiate such as fentanyl for pain control. After providing sedation, you help the student perform the shoulder reduction in a safe and controlled environment without adverse event. Clinical Application: At this time, evidence seems limited in the benefits of ketofol. However, the combination of propofol and ketamine are being researched in other settings such as transporting psychiatric patients in the prehospital environment versus using ketamine alone in the acutely agitated patient. Although there does not appear to be adverse events in ketofol, as demonstrated in this study and in others, combining two medications means that providers using this combination must be careful and use caution to reduce the risk of complications. What do I tell my patient? When it comes to painful procedures, we have different ways in managing both your pain and the way we let you sleep in the procedure. We will use a medication called propofol that allows you to sleep through the procedure. Another medication we can add is called ketamine which helps both with sleeping and pain. Both work quickly and leave the body quickly. Instead of ketamine we can use other pain medications such as morphine or fentanyl which will work differently on your body but should also help with the pain. Conclusion: Thank you for listening to the podcast and reading the blog. Please let me know if there is anything we need to change or improve. We really want to do whatever we can to make this the best project. Please e-mail us at [email protected] or see us at Twitter or Facebook. For more information on ketamine and propofol go to the sites linked down here and at the beginning. Remember, as the infographic shows below, there are still many benefits to ketamine, even if the combination with propofol for sedation is still up for debate. Thanks for reading the blog and watching the podcast. We hope to talk to you soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed