|
Most of us working any length of time in emergency medicine are either familiar with or perform the (extended) Focused Assessment of Sonography in Trauma (eFAST). Some keep with the original FAST exam which does not include the lungs, and we will talk more about why you want to include the lungs in a separate podcast. However, after having just returned from 2018 AASPA Conference where we taught participants about many clinically important exams, there were some details of the eFAST that simply could not be covered simply due to time. This podcast is devoted to providing some quick tips to improve your exam no matter your practice level.
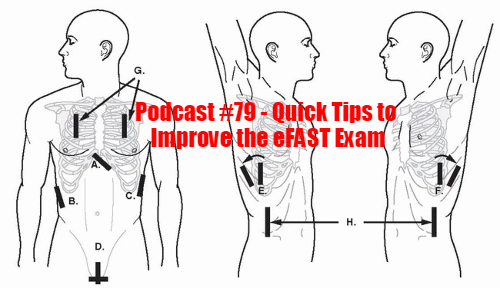
First, there are various resources to learn how to do a solid eFAST exam. The Radiological Society of North America (RSNA) released a paper just last year regarding updates in the exam. ACEP also has a nice review of the topic including some additional pearls and pitfalls. SonoMojo has a two part piece full of solid information. Family Practice Notebook has really great pictures along with nice diagrams on where to place probes with some excellent images to check out. Radiology Key also has great images and a nice diagram (which we used above) to incorporate all the views we try to obtain especially in a true eFAST. If you are like me and prefer to learn by videos, check out Ultrasound Podcast with their 30 minute video or if you want a condensed but excellent piece get the 7 minute review from 5 Min Sono (I know, a little confusing).
With all of those great resources mentioned, let us cover some pearls. First, if the patient is initially supine when they are assessed, go for the right upper quadrant (RUQ) as your first assessment. You may even need to briefly place them in Trendelenburg to encourage fluid in this location. The same can be done with the left upper quadrant (LUQ) but focus on the RUQ first since this can often be the more likely positive exam finding. Be wary of reporting a negative exam when it is actually inconclusive because you could not see all structures. In either event, do serial exams in high suspicion or acutely devolving patients. If feasible, another option is to obtain the appropriate CTs for further examination. When there is something obstructing your view that is reversible (stomach contents that can be removed by a tube or pushing bowel gas out of the way) attempt this if it does not (significantly) delay care. If someone arrives sitting upright, you may check the suprapubic view first since free fluid is more likely to be there initially versus the RUQ. This is essentially acting like a reverse Trendelenburg position and if needed to better appreciate a hemothorax or free fluid in the pelvis can attempt such a maneuver. While in that suprapubic region, check out the pubic symphysis. Currently, we mostly diagnose pelvic fractures by CT or x-ray, but ultrasound is very reasonable. Physical exam can be done but “rocking” or compressing the pelvic invites re-bleeding or worsening bleeding by disrupting clot formation. Since we already use ultrasound effectively in diagnosing fractures, we can even look at the pubic symphysis but it is not widely used yet. Using the Young & Burgess Classification, Type II and Type III anterior-posterior compression injuries will have a pubic diastasis greater than 2.5cm. We care about these since they are “unstable” fractures. Furthermore, this can potentially save a life if performing this while preparing to intubate. Identifying a pelvic fracture before paralyzing them for the intubation can reduce the risk of massive hemorrhage by having us apply a pelvic binder prior to administering paralytics. This is because inducing paralysis will cause them to no longer splint their pelvis and can result in increased bleeding. When looking at the heart, try and use the view that will allow others the most access. Usually, this is the subxiphoid approach which is particularly nice since we can usually use the same curvilinear probe that we were using on the abdominal portion for the cardiac exam. However, you can use the curvilinear probe for other cardiac views (especially apical four chamber) just as the phased array probe can be used on the abdomen. The difference is the ease and natural transition without losing time changing out probes. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
3 Comments
Aeraj Peerzade
10/23/2020 02:22:58 pm
good
Reply
Douglas
11/11/2020 03:36:41 pm
good
Reply
Usman Afzal
11/29/2020 01:32:38 pm
Good
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed