|
Every time we transfer the care of a patient, we are performing in many ways a high risk maneuver. It is so second nature to many that we do not think about the risks. However, according to the Joint Commission up to 80% of serious preventable medical errors are attributed to poorly communicated handoffs. It begs the question, how do we better transition the care of patients within the emergency department (ED).
Early on in the blog and podcast we talked about transfers of care but that was in relation to the EMS to ED and ED to EMS handoffs. Transition within the department has different elements to consider. In this post we focus on the essentials needed for a handoff within a department.
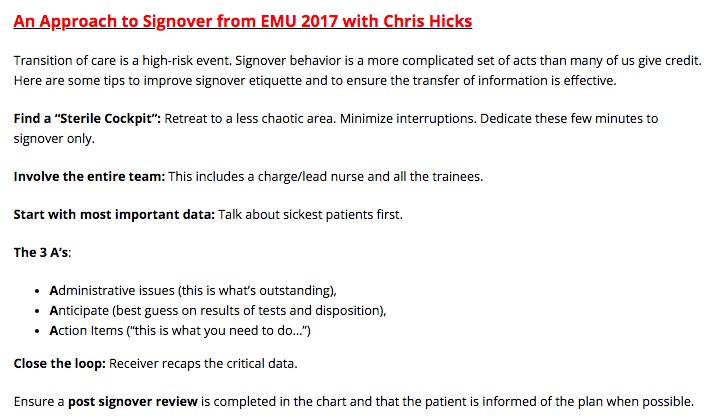
First, we must recognize that there are three aspects of transfer. There is an information, responsibility, and authority transfer. For the information transfer, this is giving the relevant data in regards to the case. This should be like any other time you are discussing a patient where you focus on the pertinent positives, negatives, management, and plan going forward. The incoming provider must accept responsibility of the patient’s ongoing care. Finally, they also accept the primary authority over the continued care going forward until another transition of care occurs. There are serious barriers to effective transfers of care. One very common issue is the amount of information given. There is a fine balance between being concise and being complete in the amount of information given. Often this is compounded by the issues of a busy emergency department and trying to get through key information while managing the volume and acuity. It is important when sharing this information to make sure that both parties are fully invested and listening. This leads to another very common and concerning barrier: cognitive bias. Four common types are triage cueing, diagnosis momentum, framing effect, and ascertainment effect. Triage cueing is something we often see and being that it occurs early in the process, can sometimes be one of the biggest hurdles. This happens when a judgement made early in the patient care process impacts a particular decision. For example, when triage says that the patient has URI symptoms because they patient has a cough and chest pain rather than focusing on the chest pain being the patient’s primary complaint leading to the delayed diagnosis of a STEMI. Diagnosis momentum is when a particular diagnosis is leaned on even though other evidence may suggest the contrary. When a presentation is made a particular way, framing effect is seen and can also impact decisions. Finally, ascertainment effect is when our thinking is impacted by expectations that already exist. The last barrier regards failure to transfer authority. This can happen when there is a failure to clearly define when the patient’s care has been handed over. After sign-out, if the previous provider stays in the department this could lead to confusion on when care has been transferred. The other issue is when the receiving provider avoids getting involved even when the other provider had already left. When performing a handoff there are essentially three stages: pre-turnover, meeting, and post-turnover. Pre-turnover is when the provider leaving prepares by organizing and reviewing plans. The meeting would be the actual handoff to the new provider. The post-turnover is when the new provider acts of the information provided. A standardized method of transitioning care can be helpful, but it has to have the right steps. Although there is no perfect solution, there aresome key steps that need to be taken to improve the transition of care. First, is to review the current information and pre-round on patients. This can help tie up loose ends and let people know you are about to leave. During the meeting phase of the handoff, try to round together. Both stages of rounding should optimally be at the bedside, especially for high risk patients. Sometimes, patients staying in the department who have already been departed or admitted and just waiting to leave the physical department may not need this level of care, but should still be considered. Next, relay to the rest of the team that the handoff has occurred. This helps avoid the issue with transfer authority. Also, it may allow for updates to occur such as new information that nursing has on the patient. Finally, receive feedback by reviewing any questions or suggestions regarding care. Like any other high-risk element of our shift, there should be minimal interruptions. Thanks to Anton Helman (for the graphic) and Chris Hicks (for the method), there is a nice approach to handoffs that came from Emergency Medicine Cases Episode 99.
Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
3 Comments
EC PCRMC
3/8/2018 07:49:49 am
Great discussion.
Reply
Chip Lange, PA-C
3/8/2018 09:11:25 am
Thank you. Glad you enjoyed it.
Reply
5/6/2022 05:07:32 am
<b><a href="https://www.dosepharmacy.com/fildena-25mg-tablet">buy fildena 25 mg online</a></b> will not make you come or prevent premature ejaculation. It is primarily an erectile dysfunction medication and does not directly impact time to ejaculation. It is not usually prescribed to treat premature ejaculation.
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed