|
There is also some source of news out there that is contributing to misinformation. As we have talked about before, misinformation is a daily presence but usually we can quickly fact check a source. Most of these are from sources where the credibility is already questionable. However, what happens when a major media source misrepresents information in a way that is potentially damaging to medicine and the patients we care for?
Before we dive too far in the topic, a quick announcement. The AAPA Board of Directors 2018 Election is happening now. It opened on April 6, 2018 and will close April 16, 2018. If you are an AAPA member and have not yet voted you need to do so quickly! This is a major year and your vote matters. Now back to the clinically related discussion for today.
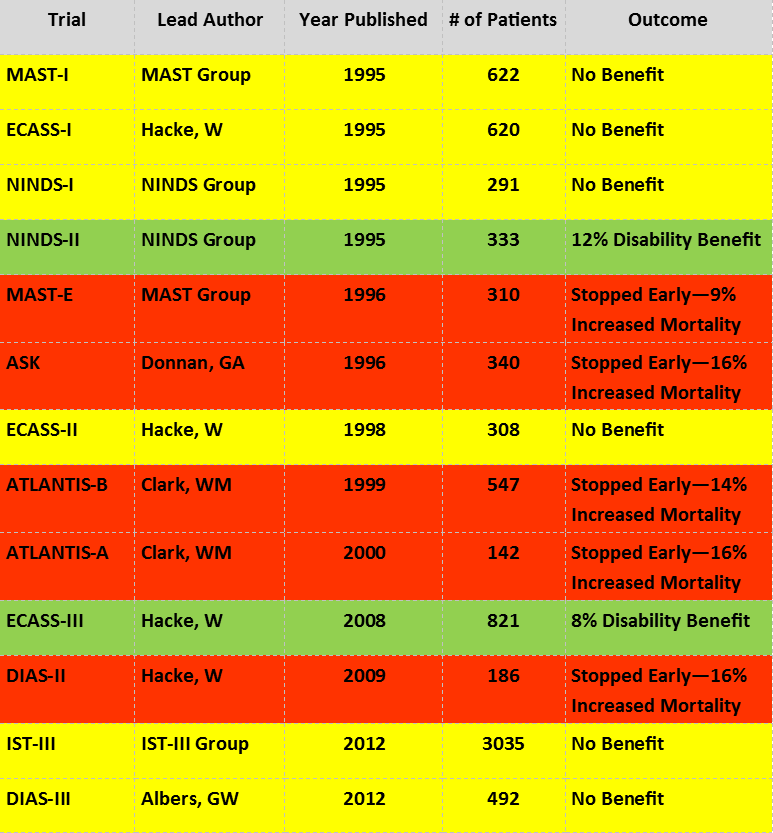
The issue we referenced is in regards to a recent New York Times publication by Gina Kolata who published two articles on March 26, 2018. There was a little delay but since those publications the #FOAMed world has caught wind of the articles. The “Times Insider” piece titled “A Medical Tip’s Unexpected Outcome” is about how Gina Kolata “debunked” a “tip” regarding tissue plasminogen activator (tPA). She reports an anonymous Canadian emergency medicine physician emailed her to explain the limitations and potential dangers of this medication. She goes on to explain how she had previous knowledge of the medication and knew of its benefits. In that publication she compares the claims of its negative impact as “fake news” by those concerned with the limitations. She then goes on to explain that she wrote her other article built off of the story about the father of a researcher in tPA who ultimately had a stroke and did not receive this medication. This is when the story truly gets interesting for a number of reasons. The article, “For Many Strokes, There’s an Effective Treatment. Why Aren’t Some Doctors Offering It?” heavily implies that this is a closed case. As we will discuss more momentarily, this is very far from the truth. The story is built around Christopher Lewandowski who is an emergency medicine physician in Detroit, Michigan and helped in the original study. He was chosen for the piece specifically because he feels his father was harmed by not receiving tPA for his stroke. However, it almost entirely ignores the discussion of the risks. There are also claimed facts in the articles without citations such as a claim that “up to 30 percent of stroke victims who arrive at hospital on time and are perfect candidates for the clot-buster do not receive it.” It then implies that those not receiving it are then destined to permanent disability which would have been prevented by tPA. It also talks about how “rates of cerebral hemorrhage have declined as doctors have gained experience over the years” but again lacks a related citation. Although the article does briefly talk about the risk of bleeding, it fails to talk about the number needed to treat (NNT) or the number needed to harm (NNH). Although calculations on the NNH vary, it is usually 1 in 17 to 1 in 20 leading to symptomatic intracranial hemorrhage and/or mortality compared to those who did not receive this medication. This means that 5-6% of people who receive tPA will develop a bleed and/or die. Finally, and quite possibly the most intriguing part, is the direct attack on #FOAMed and attacking the spread of knowledge through social media versus other (paid) methods such as journals or conferences. Let us not forget, there are predatory journals that exist and previous stings have demonstrated that these are not peer reviewed (at least not well). When it comes to peer review, blogs and podcasts may not receive it in the traditional sense but it does happen and has the benefit of happening in real-time. They talk about how young learners are not reading the articles or practice guidelines but are citing blogs and podcasts. Although this can very well happen, as almost anyone in the #FOAMed world will tell you, it is extremely important to go to the information directly and research. The information we provide is meant to help supplement and help digest the often dense data that is present in articles and guidelines. Let us talk about some of these key issues starting with these guidelines. Those who performed the studies and then helped support the making of most of the guidelines are heavily influenced by pharmaceutical companies, especially in the case of stroke care and thrombolysis. It is important when discussing how something is being decided to not only look at the evidence but who is pushing the data and their potential biases. Although the bias may not be intentional, it is a real threat to the legitimacy of research and appropriate adoption. The American College of Emergency Physicians in 2015 did update their guidelines and did so where “There were no relevant industry relationships disclosed by the subcommittee members” which is very different than most other groups. They were not able to make any Level A recommendations but did make Level B and C recommendations. This matters for a number of reasons but ultimately they talked about how tPA “should be offered and may be given” to select patients within three (3) hours of symptom onset and that “tPA may be offered and may be given to carefully selected patients” within 3 to 4.5 hours after symptom onset in appropriate centers. In both cases, shared decision making is encouraged when feasible. The reason why this matters is that the liberal language allows for more careful consideration based on the complex nature of this disease process to help tailor care to individual patients. It was quickly mentioned in the New York Times articles how there are more articles that demonstrate harm compared to benefit. Of the thirteen (13) main trials frequently cited, five (5) of them were stopped early due to increased mortality. Also, the famous NINDS-II trial from 1995 that really is at the heart of this discussion has a couple of major flaws. The original primary outcome was for improvement in functional and stroke scores by 20% but was never reported and changed post-hoc to favorable versus unfavorable outcomes which led to a calculated NNT of 8 for a post-hoc “favorable” outcome. We could even discuss how the fragility index was only three (3) for this study which has its own implications but is better discussed on another site given its complexity.
We should also note that the ECASS-III trial of 2008 (the only other favorable trial) found a NNT of 15 for “favorable” outcomes with no mortality difference. These outcomes of both of these studies are based on modified Rankin Scale (mRS) which has its own flaws including the concern for inter-observer variability.
It is worth noting that there was a Cochrane review from 2009 with an update in 2014 that had very heterogeneous data in a clinical sense. Although Cochrane discussed a 6% increase in a favorable outcome with a mRS of 0 or 1, there was also a 6% increase in symptomatic hemorrhage and/or death of 6% which means their NNT and NNH are 17. Again, it is worth reviewing this data given the many intricacies and caveats. The devil is also in the details and a nice breakdown of why the Cochrane review is potentially flawed is well discussed on EM Literature of Note along with a follow-up post regarding a meta-analysis. He actually covers tPA a lot and even has some things much more recent that we do not have time or space to cover here today. To get back to the biggest concern, the attack of #FOAMed in this article is not to be taken lightly. Like any type of information out there, we can find both the good and the bad. The goal should be to help process complicated information in a way that makes it more digestible and enhance the educational experience. Attacking an entire method of learning that has forever changed medicine is detrimental to our future. It would be akin to staying mute and only reading textbooks because talking to other people with different experiences and knowledge would be sacrilege in the house of medicine. Thanks to such technological advances of social media and the internet in general we are able to cut down the knowledge translation window in a rapid manner that helps get evidence to the bedside more quickly. There have been many detailed discussions regarding stroke care in the #FOAMed world and it would be well worth your time to see how well the information can be broken down in a manner that makes it practical. Then go back and do exactly what we ask: read the original literature and see what conclusions you come up with after critically analyzing the details. You might just be surprised. Some of our favorite sites are REBEL EM, The SGEM, EmCrit, FOAMcast, and First10EM. Health News Review also did a nice piece directly related to the New York Times articles. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||

 RSS Feed
RSS Feed