|
Mobile Stroke Units (MSUs) are ambulances that are designed to improve the time of delivery of stroke care to patients. This sounds like an excellent idea at the surface, but is the cost and approach practical?
The concept behind a mobile stroke unit (MSU) is to place a computed tomography (CT) scanner with a CT tech in a large ambulance with a mobile lab, paramedic, registered nurse (RN), and usually a neurologist in an ambulance to provide care for stroke patients on scene versus transferring immediately to a hospital for the workup to be performed. Studies can be performed in the field including a head CT with the ability to determine if tPA should be given in the field. Many now also can do CT angiography (CTA) for further investigation of a clot. The first such ambulance started running calls in Berlin in 2011 (called STEMO in Germany).
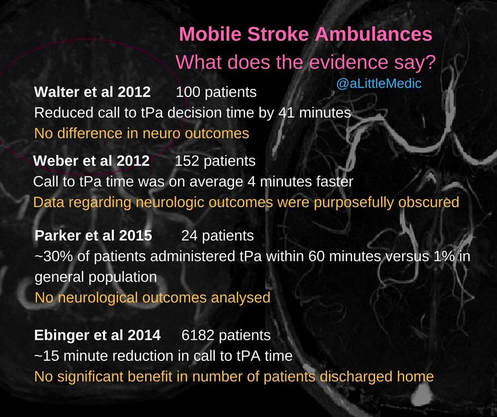
Since its inception in Germany, the United States has been pushing to do the same with the first MSU being in Houston, Texas in 2014. The approximated cost of these units is over $1 million with another $1.2 million (based on a 12 hour day) annually to keep these trucks going. This is so much an issue that in Houston the neurologist was replaced by a second paramedic and the consult is now via telemedicine. However, by doing so the CT images must be relayed to the hospital by this telemedicine link or even have to wait until the patient is at the hospital. A CTA of the brain contains approximately 3.5 gigabytes of data which makes it difficult to transmit prior to reaching a hospital in many cases. In an observational German study by Ebinger et al known as the Pre-Hospital Acute Neurological Therapy and Optimization of Medical Care in Stroke Patients Study (PHANTOM-S) demonstrated a decreased time to delivery of tPA but that patient oriented outcomes such as improvement in a modified Rankin Scale (mRS) did not exist. It is worth noting the pilot study by Weber et al did not discuss neurological outcomes and focused on times. The Cleveland Clinic’s MSU study found a statistically significant difference with their delivery of tPA but it did not report clinically significant outcomes. The same is true for the AHA Stroke Journal article by Parker et al covering Houston’s MSU program. A lack of improvement in mRS with MSUs compared to conventional care has also been found in a trial from Berlin with Kunz et al and with Walter et al in 2012 also from Germany (both were published in Lancet Neurology). Then there is the reimbursement. If the average trip by truck is approximately $500, the payouts from tPA and thrombectomy which can be varied but are calculated at $12,000 and $30,000 in reimbursements, respectively. Going back to our estimated annual costs for a 12-hour a day program, tPA would need to be administered approximately 100 times annually to be cost-effective. To be more accurate with that number, this would need to be 100 patients who would otherwise have not received the medication and therefore reimbursement would not already happen. This does not factor a number of other variables such as if that patient would then be eligible for thrombectomy when they otherwise would not or for paying the costs of the ambulance originally. As was evidenced in the BEST-MSU study during its run-in phase, they averaged tPA treatment 1.5 times a week. This means it is getting less than the 100 patients goal (again assuming those patients otherwise would not have gotten tPA. It also does not factor if these patients even need tPA as they may have resolving symptoms which usually indicated a transient ischemic attack (TIA) which would not need tPA. We also have to keep in mind that these ambulances are usually serving a small geographic region. They are located in cities and close to their stroke centers. Although they have a statistically significant improvement in time to tPA delivery, this has not necessarily translated to patient oriented outcomes. This essentially means that the vast majority of patients out there are not receiving benefit from a very expensive service and could better benefit from education and training that would benefit the larger number of patients. Something as simple as teaching EMS how to perform more thorough neurological exams (as we have discussed before) which can be performed in a couple of minutes is of little to no cost. By EMS having more tools to properly recognize stroke-like symptoms, the proper activation can be in place without the expensive and overall unproven equipment.
There is an infographic made by Aidan Baron regarding some of the evidence on mobile stroke units. Keep in mind though we covered and have linked even more studies than those mentioned there but they have essentially the same points.
One last thing to mention. If you feel that mobile stroke units are becoming an issue as we have discussed, get out on social media like Facebook and Twitter to let your thoughts be known using the #StopCTambulances or the #StopTheCTambulances hashtag. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on iTunes. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed