|
Scaphoid fractures are often missed but important fractures due to their potential complications including non-union, post-traumatic osteoarthritis, and potential for avascular necrosis (AVN). These complications can even lead to lawsuits which further emphasizes the need to identify and properly treat these fractures whenever possible.
This topic is in part thanks to feedback by readers and listeners such as yourself. One such person reached out to tell us how much he appreciated our previous posts including one on tibial plateau fractures (one topic that was requested multiple times). He wanted us to cover more orthopedic topics and scaphoid fractures has been another one that has been requested. This feedback is important to us and will help us continue to grow in our ability to serve you and help you continue to grow as a clinician.
Let's start diving into the content. As mentioned in the title, we are going to cover 5 pearls that you should know with scaphoid fractures. While there are many sources of great content to cover this topic, a recent BMJ article titled Fractures of the Scaphoid by Berber et al. published on May 27, 2020 does an excellent job and is also the source of our images below.
#1 - Fractures that are not promptly diagnosed or treated can progress to non-union.
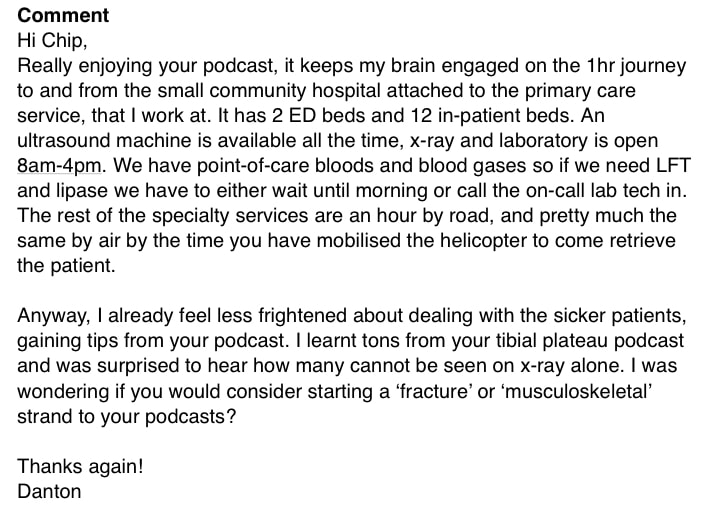
Surface markings of (a) the anatomical snuff box (yellow triangle) and (b) the scaphoid tubercle. The trapezial ridge is also indicated to highlight the close proximity of the two anatomical features. (c) The thumb longitudinal compression test.
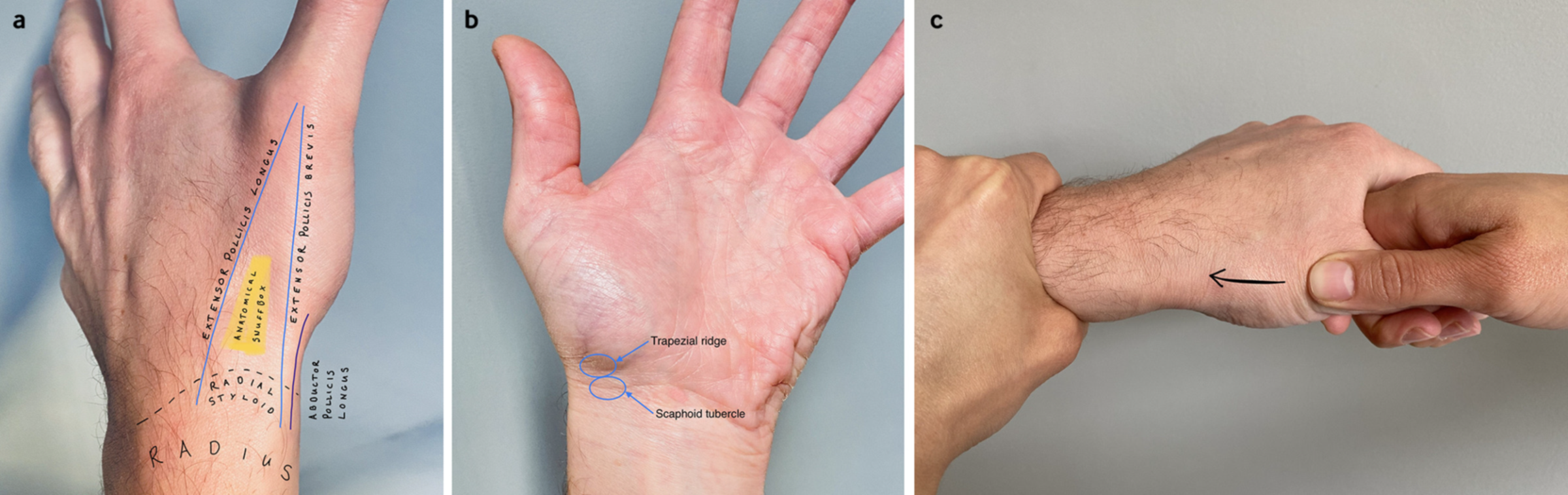
Scaphoid views performed six weeks after the injury. Three of the standard scaphoid series are presented including (a) posteroanterior, (b) pronated oblique, and (c) Ziter views. A proximal pole fracture is clearly seen on the pronated oblique and the Ziter views. The fracture is still not visible on the posteroanterior view, similar to the equivalent radiograph taken at day 1. Arrow indicates fracture site.
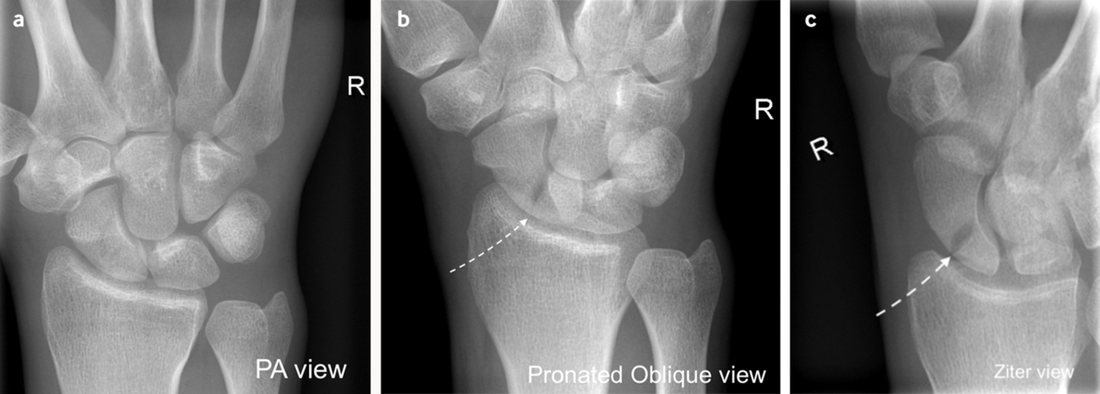
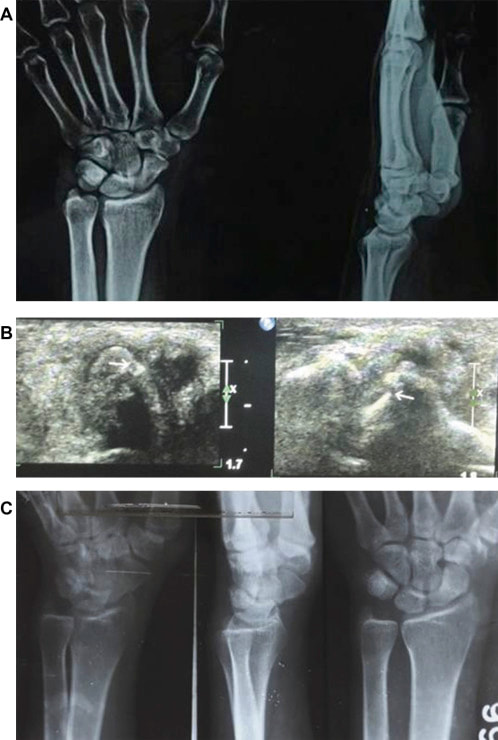
As a bit of a bonus, we are going to talk about something else to consider: point of care ultrasound (POCUS) to examine for a scaphoid fracture. It is important to know there is only a limited amount of evidence on this subject. We are going to cover it here but understand that this can be a challenging exam and one that is not widely known or taught. It could be a more common exam in the future though. Some of the earliest evidence is from 20 years ago. Five studies over the course of the next five years are discussed in aBest Bets blog post and does well discussing the studies as a quick review. A more recent review was published in2018 by Kwee and Kwee in Skeletal Radiology. The images below are from an article in the Chinese Journal of Traumatology by Jain et al. published in 2014. In that last study, the accuracy of scaphoid fracture detection by ultrasound was 98% compared to 20% with x-rays. This miss rate seems very high for x-rays compared to what is discussed above, but it is important to look at sensitivity and specificity. X-rays were 35.7% sensitive and 40% specific whereas ultrasound was 79.8% sensitive and 76.7% specific. While not great, it is still a beneficial tool that could be helpful. Even when looking at the Kwee study, the pooled sensitivity was 85.6% and the specificity was 83.3% but some smaller studies do report 100% sensitivity and/or specificity. There are many factors as to why this may be the case and it again emphasizes the need to understand there is not a perfect study.
A: Initial X-ray with normal findings. B: USG showing cortical disruption as pointed by arrow head. C: USG showing decreased width of fractured scaphoid due to impaction as compared to normal side (blue line-normal side, green line-affected side).
A: Initial X-ray with no positive findings. B: USG showing cortical discontinuity of scaphoid pointed by arrow. C: X-ray after 6 weeks showing resorption of fracture site and callus formation.
Remember to be careful with these fractures and have a low threshold to image and immobilize if there is clinical suspicion. Also educate the patient on the importance of this and help ensure appropriate follow-up for further management. If you want to learn more about ultrasound, check out Practical POCUS. They have live and on-demand courses both online and in-person. Even during the COVID-19 pandemic, Practical POCUS can provide safe and effective education for you. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on Apple Podcasts. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
1 Comment
Milton Bullard
1/6/2022 09:40:54 am
I work at a Orthopedic Outpatient Clinic. Where can I go to get the various Orthopedic and Podiatry views to be a better technologist for our patients and doctors. Your information would be highly appreciated.
Reply
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed