|
We have mentioned in previous podcasts that if you have questions or special requests to send them our way. Another one of our listeners did just this after listening to part of our ATLS series. This has been a very popular series and we are so glad you enjoy it so much. The discussions that have been built off of this as a result has led to even more great podcasts.
Podcast #215 on shock in trauma raised a lot of great questions that led to follow-up podcasts. Podcast #216 discussed the use of vasopressin in trauma and what evidence is present. Podcast #219 then talked about what volume resuscitation and how flow is a major part of deciding what vascular access could be considered the "best" in a given situation. Now the question is why would we want to use plasma first and the original question from the email is included below.
To get to the answer, we are going to take a technical dive and go over the science in detail.
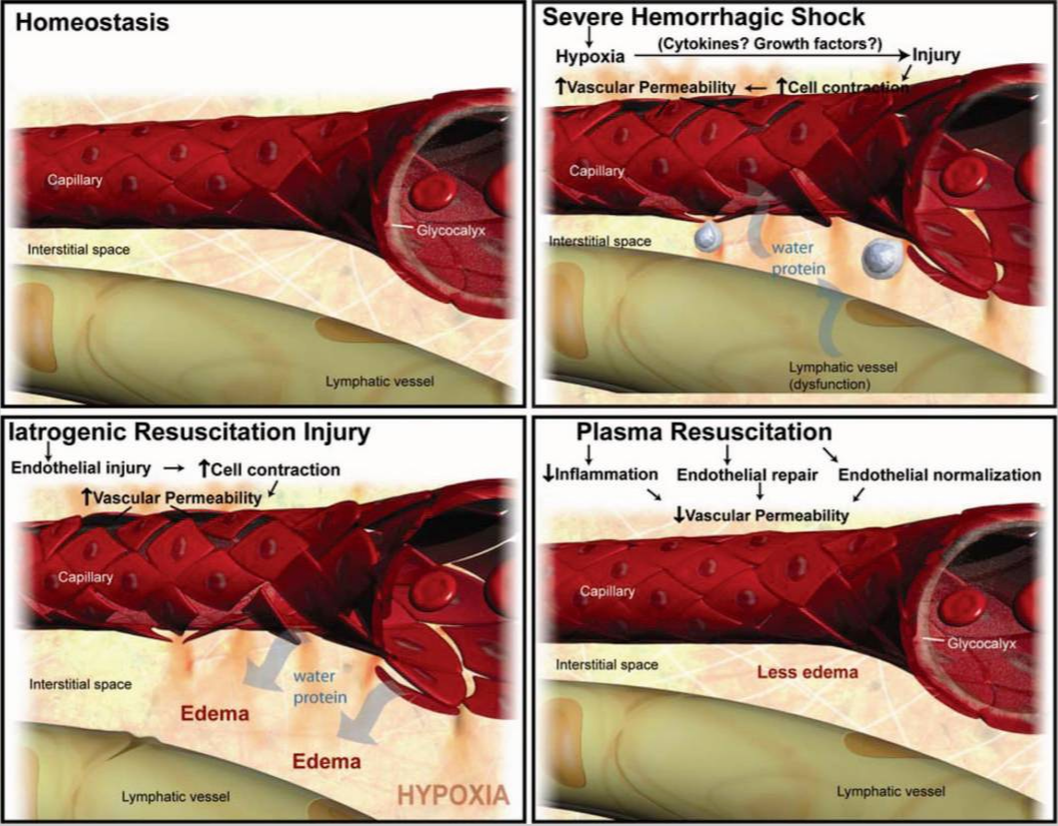
First off, it is worth mentioning that when possible whole blood should be used as it gives all the benefits of blood. However, in most cases having whole blood is simply not an option at this time. In many places, packed red blood cells (PRBCs) are given first because they are the most readily available from a blood bank. While fresh frozen plasma (FFP) may be available, it takes time to thaw. Unless there is liquid plasma available, there is usually a delay in it being available including in a massive transfusion protocol (MTP). Plasma is preferred versus crystalloids is based on what is in the plasma. While it lacks the hemoglobin for oxygen carrying capacity, it does carry many other important components simply not seen with crystalloids such as saline. There has been evidence demonstrating that resuscitating with plasma (instead of crystalloid) repairs the “endotheliopathy of trauma,” or the systemic endothelial injury and dysfunction that lead to coagulation disturbances and inflammation. While saline can improve volume, plasma can do this and address the underlying coagulopathy (at least in part since it does not have platelets). In approximately a third of patients, trauma induced coagulopathy is seen within the first 15 minutes of trauma which would be prior to resuscitation efforts. It is worth mentioning that the systemic impact of hemorrhagic shock on the endothelium has become more widely recognized. "Endotheliopathy of trauma” is a term to describe systemic endothelial injury and dysfunction that can lead to coagulation disturbances, inflammation, vascular leak, edema, and tissue injury. Plasma has a beneficial impact on endothelial permeability. When endothelial cell permeability is induced by hypoxia, thrombin, or vascular endothelial growth factor (VEGF), plasma has been shown to repair endothelial tight junctions and decrease paracellular permeability. This is something that is not seen with crystalloids and can be worsened by them. The increased permeability of the endothelium during shock states is better controlled by plasma whereas crystalloids are known to lead to significant interstitial edema and other complications such as acute respiratory distress syndrome (ARDS) and multi-organ failure.
"Working biological model of the mechanism of action of FFP. This figure depicts our working biological model of the mechanism of action of FFP. HS leads to a deviation of the vasculature from homeostasis. HS induces hypoxia, endothelial cell tight junction breakdown, inflammation, and leukocyte diapedesis. FFP repairs and “normalizes” the vascular endothelium by restoring tight junctions, building the glycocalyx, and inhibiting inflammation and edema, all detrimental processes that are caused by iatrogenic injury with fluids such as lactated ringer's solution." (From Article Cited Above)
Benefits of plasma do not just stop with the coagulation. Similar to crystalloids, plasma is iso-osmolar with blood and contains all of the cations and anions present in blood. However, this balance would be closer to the actual balance seen in blood versus the abnormalities noted in products such as saline. Like colloid resuscitation fluids including albumin or non-human polysaccharides such as large dextrans and starches, it has high oncotic pressure (28mmHg vs. 3 mmHg in saline) which helps to keep fluid in the vessels. This all points to benefits plasma has versus other fluids used in resuscitation that would not be blood products.
Essentially, plasma addresses many of the issues that arise in trauma that simply cannot be fixed with crystalloids. While crystalloids can help with volume resuscitation, it really adds nothing else meaningful and really increases the risks of complications and harm. PRBCs and platelets still matter in addition to plasma, but more trauma teams are recognizing the benefits of using plasma earlier in resuscitation. There are some great discussions out there discussing some studies including the COMBAT and PAMPer trials which REBEL EM reviewed in detail. Let us know what you think by giving us feedback here in the comments section or contacting us on Twitter or Facebook. Remember to look us up on Libsyn and on Apple Podcasts. If you have any questions you can also comment below, email at [email protected], or send a message from the page. We hope to talk to everyone again soon. Until then, continue to provide total care everywhere.
0 Comments
Leave a Reply. |
Libsyn and iTunesWe are now on Libsyn and iTunes for your listening pleasure! Archives
August 2022
Categories |
||||||


 RSS Feed
RSS Feed